Comprehensive Guide to Vitamin D Supplements
🌞 Vitamin D: The Ultimate Science-Based Guide to Benefits, Dosage, Sources, and the Best Vitamin D Supplements
✅ Welcome to the “Vitamin D Reference Page” on Pelank Supplement—where every question you’ve ever had about Vitamin D, from basic concepts to advanced decisions, finds a clear, scientific, and practical answer.
🧭 This page isn’t just an educational article—it’s a complete, trustworthy roadmap designed to help you understand whether Vitamin D is truly essential for you, what dosage fits your needs, which form is the better choice, when testing is necessary, and how to use it safely and intelligently.
🧬 In this guide, we go deep into Vitamin D—what it actually is, how it functions in your body, the key differences between D2 and D3, what IU really means, and how to correctly read supplement labels according to U.S. standards.
🧪 If you already have your blood test results (25-Hydroxyvitamin D), this guide will help you interpret your number correctly, determine whether you’re deficient, sufficient, or excessive, and understand what evidence-based and safe steps to take next.
🦴 Whether your goal is to maintain bone health, prevent Vitamin D deficiency, or manage intake alongside calcium and magnesium, this guide delivers all essential insights—clearly, practically, and without exaggeration.
🛡️ If you’re looking to improve immune function, mood, athletic performance, or reduce fatigue, this page clearly separates solid scientific evidence from unsupported marketing claims.
⚠️ If you’re concerned about side effects, toxicity, high calcium levels, kidney stones, or interactions with medications, the dedicated “Red-Flag” and “Caution Group” sections are written precisely to address those issues.
📌 Pelank’s Commitment: This article is crafted to be easily understandable for general readers while maintaining the structure, precision, and citation standards of an international-level reference—especially aligned with U.S. guidelines and standards.
✅ From this point onward, the goal isn’t just to inform—it’s to guide your decisions: Should you take it or not? At what dose? For how long? In what form? And with what safety criteria?
Vitamin D at a Glance
Pelank Supplement ©
🧬 Vitamin D (cholecalciferol) is a fat-soluble compound that can be obtained both from food/supplements and produced naturally in the skin through sunlight exposure.
☀️ When UV rays hit the skin, Vitamin D synthesis begins—meaning unlike most vitamins, Vitamin D isn’t supplied only from external sources.
🧪 After being produced or consumed, Vitamin D is first converted in the liver to 25(OH)D (calcidiol), and then mainly in the kidneys to its active hormonal form, 1,25(OH)₂D (calcitriol).
🧠 The reason it’s often referred to as a “vitamin/hormone” is because its active form, calcitriol, acts through the Vitamin D Receptor (VDR) to influence gene expression and multiple body functions—just like a true hormone.
🦴 Its most well-known classical role: enhancing calcium absorption in the intestines and maintaining proper calcium/phosphate balance for normal bone mineralization—preventing rickets and osteomalacia.
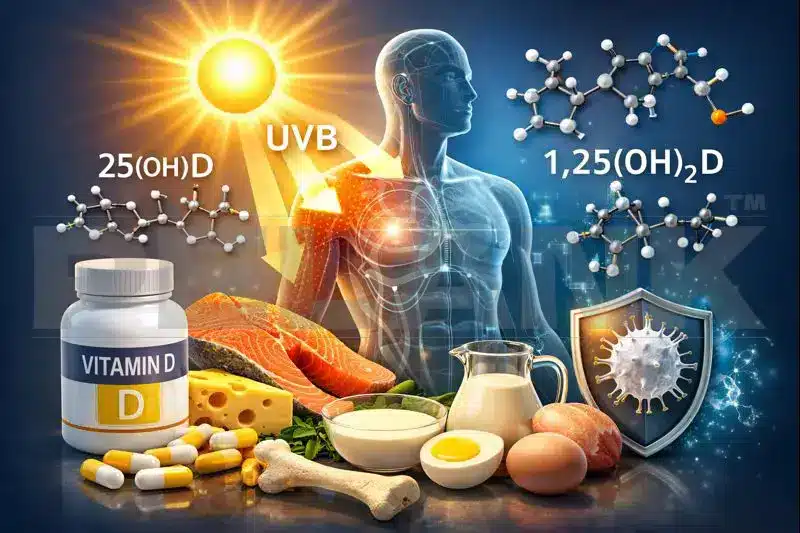
✅ The main marker used to assess Vitamin D status in blood tests is 25(OH)D, as it reflects overall input from sunlight, diet, and supplements.
✅ 1,25(OH)₂D (the active form) is not a reliable indicator of total Vitamin D stores, since it has a short half-life and is tightly regulated by hormones and calcium/phosphate balance.
✅ Vitamin D supplements come in two main forms: D2 (ergocalciferol) and D3 (cholecalciferol).
✅ In direct comparisons between D2 and D3, evidence from a meta-analysis shows that D3 is, on average, more effective at raising blood levels of 25(OH)D than D2.
✅ The most reliable and evidence-based reason to take Vitamin D is for bone and calcium-related health and correction of deficiency; “cure-all” claims don’t have consistent scientific backing.
✅ Vitamin D status isn’t solely dependent on diet—sun exposure can significantly increase 25(OH)D levels, which is why predicting one’s status based only on dietary intake can be misleading.
✅ Since Vitamin D is fat-soluble, excessive intake (especially from supplements) can cause toxicity, usually leading to hypercalcemia and hypercalciuria.
✅ Sunlight exposure alone does not cause Vitamin D toxicity, because the body has natural feedback mechanisms that limit overproduction in the skin—unlike with high-dose supplements.
✅ Vitamin D is well absorbed in the intestines, and taking it with a meal containing fat enhances absorption (though some absorption still occurs without fat).
✅ Certain medications can lower Vitamin D levels or interact with it (e.g., orlistat, some statins, corticosteroids, and thiazide diuretics), so supplementation decisions should be more carefully individualized in these cases.
✅ Who truly benefits from Vitamin D supplementation—and who might not?
🟢 Groups for whom supplementation is often more meaningful (or at least worth more serious consideration):
👤 Individuals with limited sun exposure (indoor lifestyles, long winters, or low outdoor activity).
🧴 People who receive less UV exposure to their skin (due to heavy clothing, sun avoidance, consistent sunscreen use, or living in conditions where sunlight is not a practical option).
🧑🏽🦱 Those with darker skin tones, who often require more UV exposure to produce equivalent Vitamin D levels—making deficiency more common in certain populations.
🧓 Older adults, since the skin’s capacity to synthesize Vitamin D declines with age, and lower sun exposure is also more common.
⚖️ Individuals with obesity, as studies have shown an association between higher body weight and lower 25(OH)D levels, with some evidence suggesting they may respond differently to supplementation doses.
🩺 People with fat malabsorption disorders, specific gastrointestinal diseases, or those who have undergone bariatric surgeries (like gastric bypass) are at higher risk of deficiency and often require closer monitoring and supplementation.
💊 Individuals taking medications that affect Vitamin D absorption or metabolism (such as orlistat or corticosteroids) may need dosage adjustments and periodic testing.
🟡 Groups for whom supplementation may not be immediately necessary (decisions depend more on individual circumstances):
🏃♂️ Healthy adults with balanced lifestyles, adequate sun exposure, and no clear risk factors—these individuals generally benefit more from maintaining sufficient intake and making informed decisions rather than supplementing automatically.
🥗 People who regularly consume dietary or fortified sources of Vitamin D and have no symptoms or particular risks.
🚫 Groups for whom unsupervised high-dose supplementation is unsafe and should proceed only with medical guidance:
🧫 Individuals with granulomatous diseases (like sarcoidosis or certain infections) that can lead to uncontrolled extra-renal production of 1,25(OH)₂D, increasing the risk of hypercalcemia.
🪨 People with a history or risk of kidney stones, especially if taking calcium + Vitamin D supplements together—some clinical trials have reported a higher risk, so dosage should be carefully considered.
🧠 Important note: Routine testing for everyone isn’t automatically recommended. The USPSTF states that evidence is insufficient to support universal screening for Vitamin D deficiency in asymptomatic adults—so both testing and supplementation should be based on individual risk and context.
What Is Vitamin D?
Basic but Practical Science
🧬 Vitamin D is a fat-soluble compound that the body obtains through two main pathways: production in the skin via sunlight and intake from food or supplements. Afterward, it is converted into various active forms in the body to perform its physiological functions.
🟠 Types of Vitamin D: D2 vs D3 and Their Practical Differences
🧪 Vitamin D in supplements usually comes in one of two forms: D2 (Ergocalciferol) or D3 (Cholecalciferol). Both can raise Vitamin D levels, but they’re not identical in practice.
⚖️ Comparative studies have shown that D3 is often more effective than D2—it generally raises and maintains 25(OH)D levels more efficiently and consistently (especially under similar dosing conditions).
🧠 For consumers, the practical takeaway is that if your goal is to increase and stabilize 25(OH)D levels, D3 is the more common—and usually more logical—choice, unless your doctor recommends D2 for a specific reason.
🏷️ When reading supplement labels, you may see one of the following terms:
✅ Vitamin D3 (Cholecalciferol)
✅ Vitamin D2 (Ergocalciferol)
🔍 The key point is that the actual effect is best assessed by measuring 25(OH)D in your blood—not just by what’s written on the package.
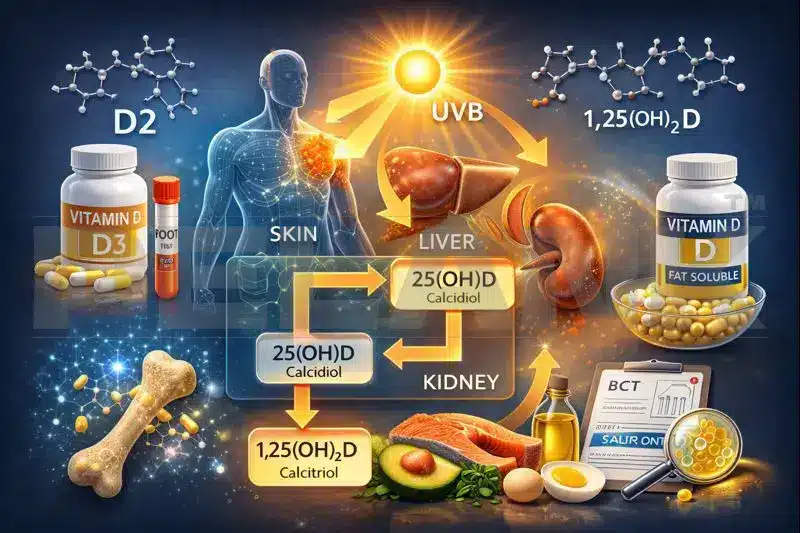
🔁 Metabolic Pathway: Skin → Liver → Kidneys (25(OH)D and 1,25(OH)₂D)
☀️ The process begins in the skin: UVB exposure triggers the conversion of precursors into Vitamin D—the body’s natural way of producing the “raw material.”
🧫 Next, the liver converts Vitamin D into 25(OH)D (Calcidiol), the main circulating form in the blood and the best overall indicator of your body’s Vitamin D status.
🧬 Then, the kidneys (and in certain cases, other tissues) convert 25(OH)D into its active hormonal form—1,25(OH)₂D (Calcitriol)—which acts like a hormone and regulates various physiological processes.
🧪 Here’s the key takeaway:
✅ To assess Vitamin D status, 25(OH)D is the marker typically measured (not 1,25(OH)₂D), since the latter fluctuates with hormonal and calcium regulation and doesn’t reliably reflect stored levels.
🥑 Because It’s Fat-Soluble: Absorption Tips (With Food/Fat)
🥗 Vitamin D is fat-soluble, meaning its absorption in the digestive system is usually improved when taken with dietary fats.
🍳 Practically speaking, the best simple advice for most people is:
✅ Take your Vitamin D with one of your main meals—preferably one that includes some healthy fats such as eggs, dairy, nuts, olive oil, or avocado.
💊 If your supplement comes as an oil-based softgel, it’s often easier to take and may support better absorption for many users. However, the key factors remain consistency, proper dosage, and smart monitoring over time.
⛔ If you have fat malabsorption issues (e.g., certain digestive disorders or specific surgeries), your absorption of Vitamin D may be reduced. In such cases, the form, dosage, and monitoring should be more carefully managed—ideally under medical supervision.
📚 Sources: [S1] [S4] [S5]
What Does Vitamin D Do in the Body?
🧬 Vitamin D is a fat-soluble compound that the body obtains through two main pathways: production in the skin via sunlight and intake from food or supplements. Afterward, it is converted into various active forms in the body to perform its physiological functions.
🦴 Bone Health and Calcium Absorption
Core Evidence Axis
🧱 Vitamin D plays its most well-established, classical role in regulating calcium and phosphate balance—helping the intestines absorb calcium more effectively and maintaining optimal calcium/phosphate levels in the blood for proper bone formation and mineralization.
🧒 Vitamin D deficiency can lead to rickets (bone softening/deformity) in children and osteomalacia (soft bones, bone pain, weakness) in adults. That’s why Vitamin D is primarily a bone health nutrient, not a “miracle supplement” for everything.

💪 Muscle, Nerve Function, and Immunity
What We Know / What’s Not Certain
🏋️♂️ Vitamin D isn’t only for bones—its receptors are found in various tissues, including muscle. Deficiency can be linked to muscle weakness and reduced performance, but that doesn’t mean every healthy person with normal levels will automatically “build stronger muscles” by taking more Vitamin D.
🧠 In the nervous system, Vitamin D plays roles in several biological processes, but many popular claims—like “guaranteed energy boost,” “definite depression relief,” or “sharper focus”—lack consistent, universal evidence. The effects often depend on factors such as deficiency status, age, underlying conditions, and study design.
🛡️ Regarding the immune system: biologically, Vitamin D does influence immune regulation. However, when it comes to real-world supplementation effects, conclusions must be precise. Large clinical trials and meta-analyses show that its role in preventing respiratory infections in the general population is small, uncertain, or limited—and any measurable benefit tends to appear mainly in specific contexts (e.g., clear deficiency or regular daily dosing with moderate amounts), not as a “guaranteed shield” for everyone.
📌 Practical summary: Vitamin D has a strong, evidence-based role in deficiency correction and musculoskeletal health; but for claims involving the heart, cancer, or “universal immune enhancement,” caution and reliance on large, well-controlled trials are essential.
🧾 Correlation vs. Causation
To Avoid Exaggerated Health Claims
🔍 Many headlines say: “Low Vitamin D is linked to [insert disease].” That statement may be statistically true, but “association” doesn’t automatically mean “causation.”
⚖️ Simple example: people who spend less time outdoors or have low physical activity often have both lower Vitamin D levels and higher disease risk for unrelated reasons—so simply raising Vitamin D alone doesn’t erase all those risks.
🧪 What actually proves an effect are randomized controlled trials (RCTs) and their meta-analyses. Many grand claims about Vitamin D, when tested in large RCTs, show no clear benefit for the general population, especially when participants weren’t severely deficient to begin with.
✅ Professional takeaway: If someone is deficient, correcting it makes sense. But if not, “miracle” promises often come from correlations, not from solid scientific proof.
📚 Sources: [S1] [S4] [S8] [S9] [S10]
Sources of Vitamin D
✅ Vitamin D can be obtained through two main pathways:
✔️ Food (natural or fortified)
✔️ Sunlight (UVB) — and for most people, a smart combination of both (without excess) is the best strategy.
🍽️ Natural and Fortified Foods
With Emphasis on the U.S. Pattern: Fortification
🐟 Strong Natural Sources
Foods That Truly Contain Significant Vitamin D
🐠 Fatty fish such as salmon, sardines, mackerel, and tuna are among the richest natural sources—and are typically listed as top options in Western and U.S. dietary guidelines.
🥚 Egg yolks provide a moderate amount of Vitamin D, and consuming them as part of a meal containing healthy fats helps with absorption.
🫀 Certain fish livers (like cod liver oil) are extremely high in Vitamin D, but since doses can easily become excessive, they should be used carefully and consciously.
🍄 Mushrooms, especially UV-exposed varieties, can provide Vitamin D (mainly as D2), though the amount varies widely depending on the type and production process.
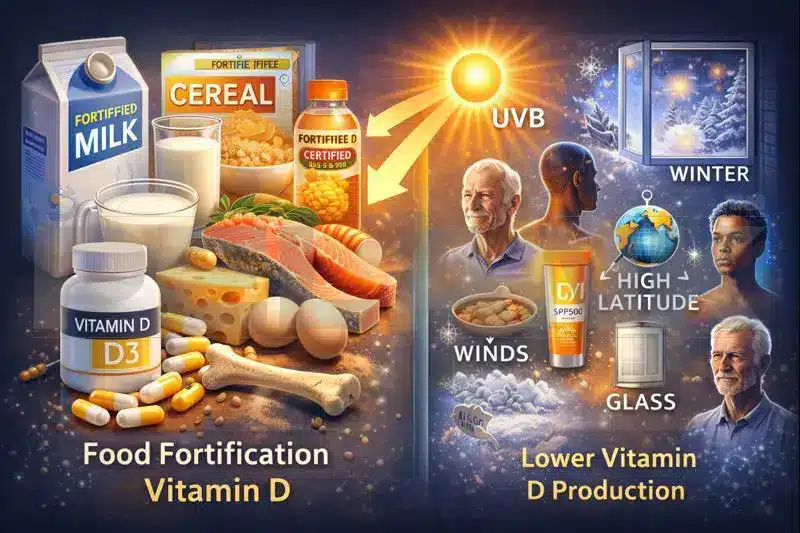
🥛 The American Model: Why Is “Fortification” So Important?
🇺🇸 In the U.S. and many other countries, a large portion of dietary Vitamin D comes from fortified foods, not just natural ones—since strong natural sources are limited and not everyone regularly eats fatty fish.
🧃 Cow’s milk is one of the most well-known fortified foods, followed by similar products such as plant-based milks (depending on the brand), breakfast cereals, some orange juices, and certain dairy products.
🧾 The Practical Takeaway: In a typical American lifestyle, someone may reach adequate Vitamin D intake without eating much fish, simply by combining a few fortified foods—but only if they read the labels correctly.
🔎 How Can You Tell If a Product Really Contains Vitamin D?
Quick Label Reading
🏷️ On U.S. food and supplement labels, Vitamin D content is usually listed in micrograms (mcg) and sometimes also in International Units (IU).
🧮 The key point: fortification isn’t guaranteed—even two similar brands may differ, with one fortified and the other not. That’s why it’s essential to always check the “Supplement Facts” or “Nutrition Facts” panel.
📌 A simple rule of thumb: if the label says “Vitamin D — X mcg (Y% DV)”, that product genuinely contributes to your daily intake. If it’s not listed, don’t count on it.
✅ Nutritional Realism: Why Food Alone Isn’t Always Enough
🥗 Even with a healthy diet, many people don’t eat fatty fish regularly—and if fortified foods like milk or breakfast cereals aren’t part of the plan, reaching sufficient intake from food alone can be difficult.
🧩 In practice, most people fall into one of two groups:
either they reach adequate levels through diet + fortification,
or they need supplementation—a decision best made based on individual risk and, if necessary, blood testing.
☀️ Sunlight: What Factors Reduce Vitamin D Production?
🌞 Vitamin D synthesis in the skin requires UVB exposure, but UVB isn’t always strong or consistent enough everywhere and at all times. That’s why relying solely on sunlight doesn’t work equally well for everyone.
🗓️ Season and Sun Angle
❄️ In colder seasons (especially fall and winter), the sun’s angle in many regions lowers the amount of effective UVB reaching the Earth’s surface—so even on sunny days, the body’s ability to produce Vitamin D can decline.
🌍 Latitude and Geographic Location
🧭 The farther you are from the equator, the less UVB radiation reaches your skin during certain times of the year. This means two people with similar lifestyles but living in different cities or countries can have very different Vitamin D statuses.
🧑🏽🦱 Skin Color
More Melanin = Harder Synthesis
🎨 Melanin acts like a natural sunscreen, filtering out UVB rays. As a result, people with darker skin tones generally need more UVB exposure to produce the same amount of Vitamin D, and populations with higher melanin levels often show greater risk of lower 25(OH)D levels—especially when combined with limited sun exposure.
🧓 Age
Reduced Skin Efficiency With Age
⏳ As we age, the skin becomes less efficient at producing Vitamin D. Therefore, older adults may generate significantly less Vitamin D from the same amount of sunlight compared to younger individuals.
🪟 Window Glass
Sunlight Without UVB
🏠 A little-known fact: sunlight that passes through window glass may feel bright and warm, but most of its UVB radiation is blocked. This means that sunlight behind glass doesn’t effectively trigger Vitamin D synthesis like direct sunlight does.
🧴 Sunscreen and Clothing
Reduced UVB Exposure on Skin
🧴 Sunscreens are designed to protect the skin and can significantly reduce the amount of UVB that reaches it. Therefore, individuals who use sunscreen consistently or wear covering clothing are likely to have lower Vitamin D production from sunlight.
⚠️ There’s an important distinction here: the goal is not to recommend unprotected sun exposure, but to understand the factors that reduce Vitamin D synthesis—so that, if needed, you can make informed dietary or supplement decisions.
⏱️ Time of Day, Shade, Pollution, and Clouds
🌥️ UVB intensity varies with time of day, cloud cover, fog/pollution, and even the sharpness of shadows. Therefore, one person’s experience with “getting sun” can’t automatically apply to everyone else.
🧩 In Summary
✅ If you fall into any of these categories—winter season, high latitude, limited sun exposure, darker skin, older age, behind windows, or consistent sunscreen/clothing use—then relying solely on sunlight for Vitamin D may not be reliable. In such cases, consider fortified foods and, if necessary, targeted supplementation.
📚 Sources: [S1] [S2] [S7]
Vitamin D Deficiency
Definition, Symptoms, and Consequences
✅ What Does Vitamin D Deficiency Mean?
🧪 Vitamin D deficiency means the body doesn’t have enough available Vitamin D to perform its key functions—especially maintaining calcium/phosphate balance and supporting bone and muscle health. Over time, this insufficiency can lead to clinical problems.
🩸 In practice, Vitamin D status is typically assessed through 25(OH)D blood testing (not the active 1,25(OH)₂D form), since 25(OH)D better reflects the body’s overall stores and status.
🧒 Deficiency in children: Rickets
Rickets
🦴 In children, prolonged Vitamin D deficiency can lead to rickets—a condition in which growing bones fail to mineralize properly, becoming softer and weaker than normal.
👶 Warning signs and symptoms to take seriously (especially in infants or children with limited sun exposure or poor dietary intake):
🟠 Slow or delayed growth in height/weight
🟠 Bone pain or tenderness
🟠 Delays in sitting, standing, or walking (in some cases)
🟠 Skeletal deformities such as bowed legs in more severe cases
🧠 The key point: rickets usually results from a persistent, long-term deficiency, not just a few weeks of low intake.

🧑🦱 Deficiency in Adults: Osteomalacia, Bone Pain, Muscle Weakness
Osteomalacia, Bone Pain, Muscle Weakness
🦴 In adults, Vitamin D deficiency can lead to osteomalacia (softening of bones), which often presents as vague, diffuse bone pain and tenderness.
💪 On the muscular side, deficiency may cause muscle weakness, reduced physical performance, and sometimes an increased risk of falls, particularly in older adults.
🚨 Persistent symptoms worth investigating include:
🔸 Diffuse bone pain (especially in the pelvis, lower back, or ribs)
🔸 Noticeable muscle weakness or difficulty climbing stairs / rising from a chair
🔸 Chronic fatigue (non-specific) combined with clear risk factors
🔸 History of low-impact fractures or decreased bone density (along with other causes)
🧱 Major Consequences of Deficiency
Why It Should Be Taken Seriously
🦴 The primary and most well-established consequence of deficiency is disruption of normal bone health—the body compensates for low Vitamin D by altering calcium regulation, which over time increases the risk of skeletal problems and bone weakness.
💪 On a functional level, Vitamin D deficiency can lead to reduced muscle performance and mobility—especially in older adults or those who are both sedentary and receive limited sunlight.
🧠 For many other claims (such as definite effects on mood, immunity, or chronic diseases), caution is warranted. It’s important to distinguish between true deficiency and taking more than your body needs.
🎯 Main Risk Factors
A Fully Practical List
🧭 If one or more of the following apply to you, your risk of insufficient Vitamin D is higher—and making informed decisions about diet, fortification, or supplementation becomes more important:
🧑🏽🦱 Darker skin tone: Higher melanin reduces Vitamin D synthesis in the skin, especially when combined with limited sun exposure.
🏠 Low sun exposure: Spending most of the day indoors, leading a sedentary lifestyle, or wearing extensive clothing coverage.
❄️ Winter and higher latitudes: Effective UVB levels are lower in many regions and seasons.
🧓 Older age: The skin becomes less efficient at producing Vitamin D, and sun exposure typically decreases as well.
⚖️ Obesity: Studies show lower 25(OH)D levels are more common in individuals with higher body weight, often requiring more tailored strategies.
🩺 Fat malabsorption or gastrointestinal disorders: Conditions that impair fat absorption can also reduce Vitamin D absorption.
🧑⚕️ Bariatric surgeries (e.g., gastric bypass): These significantly increase the risk of deficiency, so ongoing monitoring and replacement are usually necessary.
💊 Certain medications: Some drugs can reduce Vitamin D absorption or metabolism, leading to potential interactions—these situations require more careful management.
🪟 Sunlight through windows: While it looks bright, most UVB doesn’t pass through glass, so indoor sunlight cannot be relied upon as a Vitamin D source.
🧩 In Summary
🧩 If symptoms and risk factors coexist, the best approach is usually to first optimize overall intake (diet, fortified foods, lifestyle) and, if needed, add targeted supplementation.
🧪 If your risk is high or symptoms are more pronounced, a 25(OH)D blood test can help guide your decisions more precisely—but it’s not meant to be done automatically for all healthy individuals.
Blood Test and Interpretation
(25(OH)D)
✅ The Best Marker and Why: 25(OH)D
🧬 The most reliable test used to assess overall Vitamin D status is 25-hydroxyvitamin D, or 25(OH)D, because it best represents total input from sunlight, diet, and supplements over recent weeks—and it circulates in measurable amounts in the blood.
⚗️ By contrast, 1,25(OH)₂D (the active hormonal form) is not a good marker for routine evaluation, since it fluctuates with hormonal, calcium, and kidney regulation, and can sometimes appear normal—or even high—despite an actual deficiency.
📏 Common Interpretation Ranges + Unit Conversion (ng/mL ↔ nmol/L)
🧭 The key point is that cutoff values are not universal—they vary depending on the reference or guideline used. Therefore, we provide two layers here:
✅ A practical range (common in lab reports)
✅ A standard North American range (NASEM/IOM)
🧱 A very common framework used in lab reports (for quick result interpretation):
🔻 Clear Deficiency: Less than 20 ng/mL (under 50 nmol/L)
🟡 Borderline / Insufficient (depending on reference): around 20–30 ng/mL (about 50–75 nmol/L)
🟢 Sufficient for most individuals: ≥ 30 ng/mL (≥ 75 nmol/L) — this interpretation is common in certain clinical settings.
🧩 NASEM/IOM Interpretation (North American standard reference for skeletal adequacy):
🟠 The risk of inadequacy is generally considered between 12–20 ng/mL (30–50 nmol/L).
🟢 Under this framework, “nearly all individuals” with levels ≥ 20 ng/mL (≥ 50 nmol/L) are considered adequate for bone health.
⚠️ These sources also emphasize that levels above 30 ng/mL (75 nmol/L) are not always associated with extra benefit, and very high levels (e.g., > 50 ng/mL = 125 nmol/L) may raise safety concerns—depending on context and dosage.
🧮 Unit Conversion Made Easy:
🔁 nmol/L = ng/mL × 2.5
📌 Quick Reference Examples:
✅ 20 ng/mL = 50 nmol/L
✅ 30 ng/mL = 75 nmol/L
✅ 50 ng/mL = 125 nmol/L

🧫 Limitations and Variability: Why Numbers May Differ Between Labs
🧪 Measurement of 25(OH)D can vary across testing methods—some labs use immunoassays, while others rely on more precise techniques like LC–MS/MS. As a result, the same person may receive slightly different readings from different laboratories.
📉 Beyond method differences, measurement error, calibration, and even test kit variations can contribute to discrepancies—especially near cutoff values (e.g., around 20 or 30 ng/mL).
🧷 Therefore, if you plan to track your progress over time (before/after supplementation), it’s best to:
✅ Whenever possible, use the same laboratory for repeat testing.
✅ Repeat tests at reasonable intervals—not too soon—to allow for meaningful changes.
✅ Instead of obsessing over 1–2 unit differences, focus on the overall trend and clinical context.
🧾 Standardization initiatives like the CDC Vitamin D Standardization-Certification Program were created to improve test accuracy and consistency—showing that even health systems recognize this as a real challenge.
🗓️ When Should You Get Tested?
🎯 Testing is most valuable when the result will influence a decision—such as adjusting dosage, treatment duration, or confirming deficiency. Practical examples include:
🦴 If you have suspicious symptoms or signs: bone pain, muscle weakness, low-impact fractures, or evidence of bone disorders.
🩺 If you’re in a high-risk group: minimal sun exposure, darker skin with limited sunlight, older age, obesity, fat malabsorption, specific GI diseases, or bariatric surgery (e.g., gastric bypass).
💊 If you’re taking medications that affect Vitamin D absorption or metabolism.
🧑⚕️ If your doctor needs specific numbers to monitor treatment progress (e.g., after starting a prescribed dosage).
🚫 When Is Testing Usually Unnecessary?
And Why
🧘♂️ If you’re a healthy adult with no symptoms and no clear risk factors, routine testing for everyone isn’t the best use of resources—it may lead to unnecessary treatment or anxiety.
🧾 The USPSTF (U.S. Preventive Services Task Force) also states that current evidence is insufficient to recommend universal screening for Vitamin D deficiency in asymptomatic adults. That doesn’t mean testing is harmful—it means there isn’t enough data to justify it for everyone.
✅ Bottom line: Test strategically—when risk, symptoms, or clinical context suggest that “the number could change your decision.”
Who Should Take Vitamin D Supplements?
🧭 This section isn’t meant to turn you into a “lifetime supplement user.” The goal is to help you clearly and logically determine whether you actually need Vitamin D—and if so, in which scenario and with what approach.
🌳 Decision Tree
Decision Tree
🟢 Step 1: Which Group Do You Belong To?
👤 If you’re a healthy adult under 75 with no specific symptoms or clear risk factors → the main goal is to meet the RDA (Recommended Dietary Allowance) through diet and fortified foods.
If you can’t reach that target, a basic supplement that helps you meet the RDA (not high doses) is typically sufficient.
⚠️ If you’re high-risk (very limited sun exposure, darker skin + low sun, obesity, fat malabsorption, gastric bypass surgery, or certain medications) → you’re more likely to benefit from targeted testing or supplementation.
👶 If you’re an infant, child, or adolescent → ensuring daily recommended intake is important from the start (especially for breastfed infants).
🤰 If you’re pregnant or breastfeeding → there’s a defined daily need, but routine universal screening isn’t required; decisions depend on individual risk and circumstances.
👴 If you’re an older adult (especially>75+) → taking Vitamin D supplements empirically is often more reasonable and beneficial.
🧪 Step 2: Is Testing Necessary?
✅ If you have clear skeletal or muscular symptoms (bone pain, muscle weakness, low-impact fractures, or related disorders) → a 25(OH)D test is valuable because the result directly influences treatment.
✅ If you’re genuinely high-risk → targeted testing helps ensure you get the right dose and duration without over- or under-supplementing.
🚫 If you’re asymptomatic and low-risk → according to the USPSTF, there isn’t enough evidence to recommend universal screening.
In other words, routine testing for everyone has no proven necessity.
🧩 Step 3: If You Don’t Get Tested, Does Supplementation Still Make Sense?
🟡 For many low-risk individuals, if dietary intake is low, taking a low-dose supplement to reach the RDA can be a reasonable choice.
🟢 For certain groups (according to the Endocrine Society 2024 Guidelines), empiric supplementation is more commonly recommended—such as for ages 1–18, adults over 75, pregnant women, and a few other specific populations.
⛔ However, taking high doses without medical indication or follow-up is not a professional or safe decision.

🟦 Scenario 1: Low-Risk Individuals
Adequate Diet + Sufficient Sun Exposure
✅ If you’re low-risk, the main goal is to meet the recommended daily intake through a mix of natural and fortified foods plus reasonable lifestyle exposure to sunlight.
🥛 If your diet includes fortified foods (like milk or fortified dairy products), you may not need a supplement at all, or just a small supportive dose.
🧴 If you avoid the sun for skin or health reasons, your best approach is still fortified foods + low-dose supplementation, not excessive sun exposure.
🟥 Scenario 2: High-Risk Individuals
Low Sun, Darker Skin, Obesity, Malabsorption…
⚠️ If you’re in a high-risk group, two common problems occur:
🔸 Either the deficiency goes undiagnosed and persists,
🔸 Or people self-medicate with unnecessarily high doses, raising the risk of toxicity and side effects.
🧪 In these groups, targeted testing or supplementation is usually more meaningful:
🩺 Fat malabsorption, gastrointestinal disorders, or gastric bypass surgery → typically require a more precise plan and regular monitoring.
⚖️ Obesity + limited sun exposure → may lead to lower 25(OH)D levels, so guessing intake without testing can be inaccurate.
💊 Use of certain medications → can alter Vitamin D metabolism, making personalized dosing more appropriate.
🏋️♂️ Scenario 3: Athletes Athletes
Reality vs. Hype
💪 The reality: When an athlete has a genuine deficiency, correcting it can improve muscle performance, reduce weakness, and support overall recovery, since low Vitamin D is linked to poorer physical function.
🧠 The exaggeration: “The more Vitamin D, the better the performance.” For athletes with normal levels, evidence generally does not strongly support high-dose supplementation for “super performance.”
🛡️ Regarding immunity and colds: Some data suggest a potential benefit, but mainly in specific cases (like existing deficiency or consistent moderate dosing)—not as a guaranteed shield for all athletes.
📌 Practical decision for athletes:
✅ If you train mostly indoors or live in high latitudes or winter conditions, ensuring adequate intake makes sense.
✅ If you have symptoms or risk factors, a targeted test helps you supplement “not too little, not too much.”
⛔ High doses without reason pose more risk than performance benefit.
👴 Scenario 4: Seniors Seniors
🦴 With aging, both skin synthesis decreases and the risk of bone problems, fractures, and muscle weakness increases.
✅ For seniors, achieving sufficient intake becomes even more important, and several guidelines (including the 2024 Endocrine Society) emphasize a more empirical supplementation approach for adults over 75 years old.
🧩 Important Note: Older adults should not take high doses on their own, since medications, calcium intake, or kidney issues can all interact and increase risks.
👶 Scenario 5: Children and Adolescents
🍼 In infants, getting enough Vitamin D is crucial because bone growth and development are actively occurring.
✅ The AAP (American Academy of Pediatrics) commonly recommends a specific daily intake for infants—especially for those who are breastfed, as breast milk alone may not provide sufficient Vitamin D.
🧒 For children and teens, maintaining the minimum daily intake is important mainly for preventing rickets and deficiency.
📌 Practical takeaway: In children, the focus should be on meeting the recommended intake, not experimenting with high doses.
🤰 Scenario 6: Pregnancy and Lactation
👩🍼 During pregnancy and breastfeeding, the mother’s body needs enough Vitamin D for both her own health and that of the developing baby.
✅ The ACOG (American College of Obstetricians and Gynecologists) notes that pregnant women should meet the recommended daily intake, but current evidence does not support universal screening for all. Testing should be based on individual risk and circumstances.
🧪 If a deficiency is diagnosed during pregnancy, ACOG notes that many specialists consider daily doses of 1,000–2,000 IU to be generally safe, though the final decision should always be made by a healthcare provider.
Vitamin D Dosage
RDA, UL, and Therapeutic Dosing
🧭 This section is designed to clarify what an “appropriate dose” really means—the difference between the Recommended Dietary Allowance (RDA) and the Tolerable Upper Intake Level (UL), and why therapeutic doses for deficiency correction should be used thoughtfully and preferably under professional supervision.
✅ RDA by Age
Recommended Dietary Allowance
📌 The RDA is “the amount sufficient for most healthy individuals” — its goal is to cover daily needs, not to treat a severe deficiency.
🧮 Label Tip: 1 microgram (mcg) = 40 International Units (IU).
🧑⚕️ Age Group / Condition | ⛔ UL (mcg/day) | ⛔ UL (IU/day) |
|---|---|---|
👶 0–6 months | 25 mcg | 1,000 IU |
| 👶 7–12 months | 38 mcg | 1,500 IU |
🧒 1–3 years | 63 mcg | 2,500 IU |
🧒 4–8 years | 75 mcg | 3,000 IU |
🧑 9–18 years | 100 mcg | 4,000 IU |
🧑🦱 19 years and older | 100 mcg | 4,000 IU |
🤰 Pregnancy & Lactation | 100 mcg | 4,000 IU |
🛑 Safety Note: Consistently exceeding the UL—especially through supplements—can raise the risk of hypercalcemia and kidney complications. With Vitamin D, “more” is not better.
🎯 Different Goals: Maintenance vs. Repletion
Maintenance vs. Repletion
🟢 Maintenance means you either don’t have a deficiency or you’ve already corrected it and simply want to keep your level within the healthy range.
🥗 In this case, the focus should always be on fortified foods and dietary sources, adding a low-dose supplement if necessary (the goal: meet the RDA, not approach the UL).
🟠 Repletion means there’s a true deficiency or high likelihood of one, and the goal is to raise 25(OH)D levels effectively and measurably.
🧑⚕️ In this scenario, some clinical guidelines recommend short-term higher-dose protocols (for several weeks) followed by a maintenance phase.
⚠️ Critical emphasis: This phase should ideally be medically supervised and goal-oriented, since high doses used incorrectly can be dangerous and require follow-up testing.
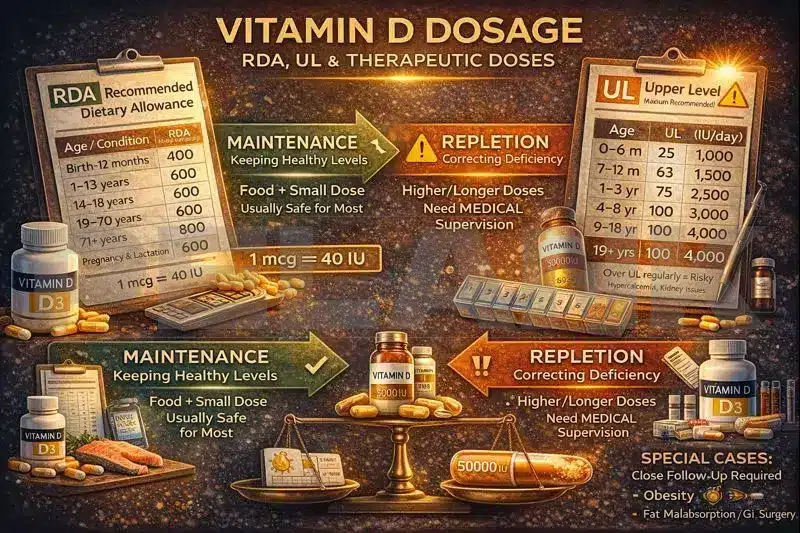
📆 Daily vs. Weekly / Monthly Dosing
Pros, Cons, and Why to Avoid Unnecessary Bolus Doses
🗓️ Daily dosing typically provides more stable blood levels and is physiologically simpler and more predictable for most people.
📅 Weekly dosing (using an equivalent total amount) can improve adherence for some, which is why it’s sometimes used in deficiency correction protocols—but still, it must be targeted and structured.
📦 Monthly or yearly mega-doses are usually not recommended, as they cause large fluctuations (spikes and drops), and some studies have linked very high annual doses to an increased risk of falls and fractures in older adults.
🚫 Practical takeaway: Avoid large, infrequent bolus doses without a valid reason or medical supervision—especially in older adults.
🧩 Dosage in Special Conditions + The Need for Lab Follow-Up
Reality vs. Hype
⚖️ Obesity
🧠 In people with obesity, many studies have shown lower 25(OH)D levels, and reaching the same target range may require a more individualized dosing plan.
🧪 The best approach for this group is not to guess with high doses, but to make data-driven, test-based adjustments with proper follow-up.
🩺 Fat Malabsorption / Gastrointestinal Disorders / Bariatric Surgery (e.g., Gastric Bypass)
🚧 In malabsorption conditions, standard doses may not be absorbed effectively; treatment must be personalized, and lab monitoring becomes essential to ensure safe correction.
💊 Certain Medications
⚠️ Some drugs can alter Vitamin D absorption or metabolism; in such cases, decisions should follow a “risk + test + follow-up” approach—not unsupervised high-dose use.
🔁 Lab Follow-Up (When Targeted Dosing or Therapy Begins)
🧪 If your goal is to correct deficiency or you’re taking higher-than-maintenance doses, your 25(OH)D should typically be retested after a reasonable period to confirm that levels are adequate—but not excessive.
Which Form of Vitamin D Supplement Is Best?
🧭 Choosing the “best” Vitamin D supplement isn’t just about the name—it depends on your goal (maintenance vs. deficiency correction), individual condition (malabsorption, obesity, age), and dosage form (drops, softgels, tablets, etc.). This section helps you make a choice that’s both effective and low-risk.
🟡 D3 or D2?
Practical Summary + Overall Evidence
🧪 The two most common supplement forms:
✅ Vitamin D3 (Cholecalciferol)
✅ Vitamin D2 (Ergocalciferol)
⚖️ Practical conclusion from evidence: Both forms can raise 25(OH)D, but in many comparative studies, D3 tends to increase and maintain 25(OH)D levels more effectively and consistently than D2.
That’s why in the U.S. market and most clinical recommendations, D3 is considered the first-line choice for general use.
🧠 So, the best choice for most people is usually:
✅ If your goal is maintenance or correction of mild deficiency → go with D3.
🟡 If for any reason (e.g., availability, prescription form, or dietary restriction) you take D2, that’s fine—it still works, but the response may be less stable, so closer monitoring is reasonable, especially when treating a deficiency.
🌱 Important note for vegans: Traditional D3 is typically animal-derived, but Vegan D3 (from lichen) is now widely available—so being vegan doesn’t automatically mean you must use D2.
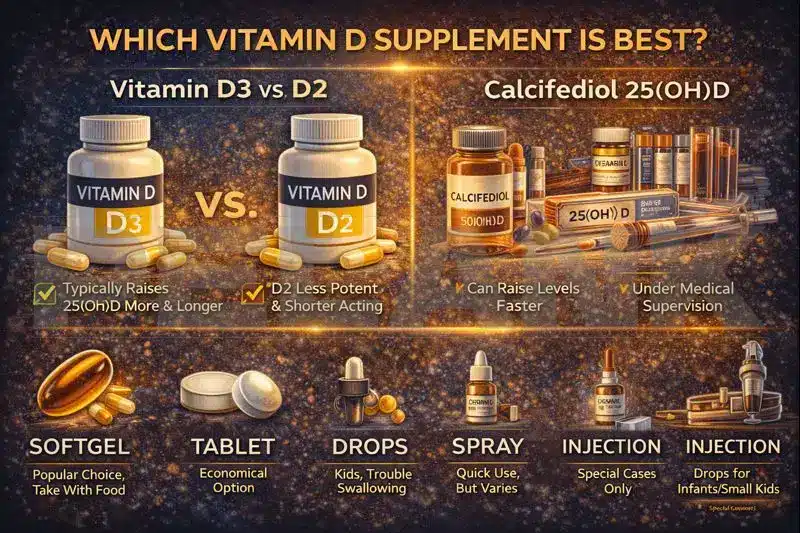
⚡ Calcifediol (25(OH)D): Why It’s Sometimes Considered “Stronger”
🧬 Calcifediol is actually 25(OH)D itself—the same form your liver naturally produces from Vitamin D.
🚀 Why it’s considered stronger/faster:
✅ Because it bypasses one metabolic step—instead of your body first converting Vitamin D into 25(OH)D, you’re directly taking 25(OH)D itself.
📈 As a result, in many situations it can raise blood 25(OH)D levels faster and sometimes achieve a greater increase with lower doses.
🧩 So, who is this form typically best suited for?
🩺 Individuals who need to correct low 25(OH)D levels more quickly or those who don’t respond well to standard D3.
🚧 People with fat malabsorption or specific clinical conditions, under a doctor’s supervision.
⚠️ Since it can raise levels faster, the risk of overshooting (excess levels) is higher if used without purpose or monitoring.
Therefore, Calcifediol is generally a professional-use option, not a first-line choice for unsupervised self-supplementation.
💊 Supplement Forms: Softgel, Tablet, Drop, Spray, Injection
When to Use Which
🟠 1) Softgel (Oil-Based)
🥑 Usually the most popular daily form, since Vitamin D is fat-soluble, and oil-based softgels provide consistent absorption and ease of use.
✅ Best for: most adults, maintenance, daily or weekly use.
⚠️ Tip: take it with a meal, preferably one containing some healthy fat.
🟡 2) Tablet
💊 In terms of effect, tablets can be just as effective if taken regularly and at the correct dose.
✅ Best for: those who don’t prefer softgels or want a more economical option.
⚠️ Note: some individuals may experience digestive sensitivity or personal preference issues, which influence the choice.
🔵 3) Drops
👶 A common choice for infants and children, as dosing can be adjusted more precisely.
✅ Best for: infants/children, people with swallowing difficulties, or anyone needing exact dose control.
⚠️ Important note: The number of drops and concentration vary between brands—always follow the label instructions carefully.
🟣 4) Spray
🌬️ Often marketed for convenience; however, product quality and absorption data vary.
✅ Best for: individuals who have trouble swallowing pills or simply prefer spray-based delivery.
⚠️ Tip: Choose trusted brands with quality control, and don’t expect “miracle absorption” claims to hold true without evidence.
🔴 5) Injection (Ampoule / Injectable Form)
💉 Typically reserved for specific medical cases and prescribed by a doctor—for example, when adherence is poor or targeted therapy is required.
✅ Best for: clinical or prescription scenarios, or certain medical conditions where a doctor decides it’s appropriate.
🚫 Critical note: Injectable doses can be very high and carry risks of fluctuations or excessive levels—never self-administer without supervision.
🧩 Which One Should You Choose?
Quick Summary
✅ If you’re an adult aiming for adequate intake → D3 softgel or tablet, taken regularly.
✅ If it’s for a child or infant → drops, following precise dosing instructions.
⚠️ If you have malabsorption, medical conditions, or severe deficiency → the form (Calcifediol, injectable, or specialized dosing) should be determined by a healthcare professional.
Better Absorption of Vitamin D
Practical Tips
🥑 With a Fatty Meal?
Yes, Because It’s Fat-Soluble
🍽️ Vitamin D is a fat-soluble vitamin, meaning it’s absorbed better in the intestines when some dietary fat is present. Therefore, the simplest practical advice is:
✅ Take your Vitamin D supplement with one of your main meals—preferably a meal that includes a bit of healthy fat.
🥚 Good examples: eggs, dairy, fish, nuts, olive oil, avocado, or peanut butter.
🧠 Key point: your meal doesn’t have to be “high-fat”—as long as it’s a real meal with some natural fat content, it’s usually enough.
💊 Oil-Based Softgel vs. Tablet
🫒 If your supplement is an oil-based softgel, it’s often easier to take and well-tolerated; but if you have tablets, that’s fine too—the most important thing is to take it consistently and with food.
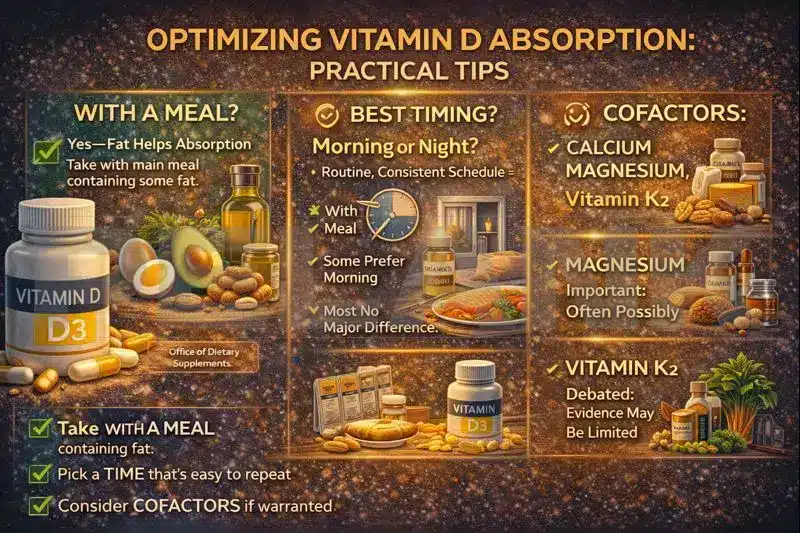
⏰ Timing (Morning/Night) and Meal Interaction
When Is the Best Time to Take It?
🕘 The practical truth is: for most people, the “best time” is whenever you can take it consistently—daily or weekly.
✅ Because Vitamin D has a long half-life, the difference between morning and evening intake usually doesn’t matter much; consistency matters more than timing.
🌙 Still, a few helpful notes:
🍽️ If you take Vitamin D with food, choose a meal you eat most consistently—for example, lunch or dinner.
🛌 Some people report that taking it at night affects their sleep (while for others, it makes no difference). This isn’t universal—if you notice any discomfort, simply switch to morning or midday.
☕ If your breakfast is very light and low-fat, it’s better to take your Vitamin D with the next meal instead.
🚫 Meal Interactions:
✅ The main real interference is taking it on an empty stomach with no fat, which can reduce absorption.
⚠️ If you’re on fat-blocking medications (like Orlistat), take Vitamin D at a different time as advised by your doctor or pharmacist.
🧩 Cofactors: Calcium, Magnesium, Vitamin K2
Proven vs. Potential
🦴 Calcium: Proven and Logical
But Only When Needed
🥛 The relationship between Vitamin D and calcium is clear—Vitamin D enhances calcium absorption, and both are vital for bone health.
✅ If your diet is low in calcium (for example, limited dairy or calcium-rich foods), adding calcium along with Vitamin D may make sense.
⚠️ But this doesn’t mean everyone should take calcium supplements; if you have a history of kidney stones or are using high-dose Vitamin D, the decision should be individualized.
⚙️ Magnesium: Important and Likely
But Not a Universal Rule
🧠 Magnesium plays a role in many biochemical reactions and is also involved in several pathways related to Vitamin D metabolism.
🟡 However, the more accurate takeaway is this:
✅ If you have a magnesium deficiency or your dietary intake is low, correcting magnesium levels can be helpful—but for most people, it’s not mandatory to take magnesium alongside Vitamin D.
🥜 Professional approach: prioritize dietary sources first (nuts, legumes, whole grains, vegetables), and if signs of deficiency appear, make a targeted decision rather than supplementing automatically.
🧡 Vitamin K2: More Controversial
No Strong Evidence for Universal Necessity
🧩 The common claim about Vitamin K2 is that it helps direct calcium to the bones and prevents vascular calcification.
🟡 The reality: K2 does have biological roles, but the idea that “everyone must take K2 with Vitamin D” is not a universally proven or mandatory recommendation.
✅ If your diet already includes sources of Vitamin K (like leafy greens or certain fermented foods), you’re likely covered.
⚠️ If you take anticoagulant medications such as warfarin, Vitamin K2 can interfere—so any changes should always be made under medical supervision.
✅ Quick Checklist
Most Practical Version
🍽️ Take Vitamin D with a meal (preferably one containing some healthy fat).
📅 Choose a time of day that helps you stay consistent with your routine.
🦴 Take calcium supplements only if your intake is truly low—not automatically.
⚙️ Magnesium “may help” if you have a deficiency or low dietary intake.
🧡 Don’t treat K2 as a “universal must-have”; be especially cautious if you’re taking blood thinners.
📚 Sources: [S1]
Claimed Benefits of Vitamin D
Facts vs. Evidence Boundaries
🧯 This section has one clear goal: to separate “proven effects” from “reasonable hopes” and “marketing claims”—so we neither idolize Vitamin D nor undervalue its real role.
🧠 The key idea: many of the bold claims about Vitamin D come from observational studies (statistical correlations), while the gold standard for proving real effects is randomized controlled trials (RCTs) and their meta-analyses.
🦴 Bone / Osteoporosis: Stronger Evidence
The Core Focus of Vitamin D
🦴 The classic role of Vitamin D in calcium absorption and bone health remains the strongest and most consistent area of evidence.
🧱 In practice, Vitamin D shows its greatest value when the goal is preventing or correcting deficiency, since low levels can lead to problems like rickets, osteomalacia, and muscle weakness.
🧩 Important note: For optimal bone outcomes, simply raising your Vitamin D number isn’t enough—adequate dietary calcium, age, fall risk, and overall bone health also play major roles.
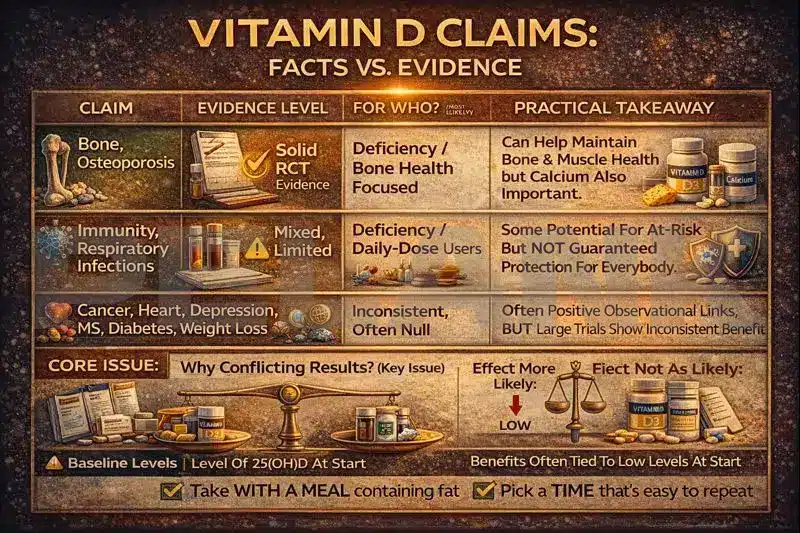
🛡️ Immunity and Respiratory Infections
What We Know / What We Don’t
🧪 Biologically, Vitamin D is involved in modulating parts of the immune response. But the key question is: “Does Vitamin D supplementation significantly reduce respiratory infections in real life?”
📉 Evidence from RCTs and meta-analyses generally shows that if there is any benefit, it’s small and context-dependent, not a universal shield against infections.
🧩 A recurring finding across studies is that the strongest benefits—if any—are seen in those with low baseline levels (true deficiency) and consistent daily/weekly moderate dosing. For people with already adequate levels, expecting a “dramatic immune boost” isn’t realistic.
🚫 What remains unproven: that Vitamin D supplementation in healthy individuals with sufficient levels can reliably prevent infections or substantially improve general immunity.
🧬 Cancer, Heart Disease, Depression, MS, Diabetes, Weight Loss
Fair Summary of the Evidence
🫀 Cardiovascular health: The large VITAL trial in the general population found no clear or conclusive benefit for major cardiovascular outcomes—so “Vitamin D for heart prevention for everyone” is not a strong claim.
🎗️ Cancer: In the same VITAL trial, no definitive reduction in overall cancer incidence was seen. Some secondary or subgroup analyses suggested potential effects on certain outcomes, but these are not strong enough for universal conclusions and should be interpreted cautiously.
😔 Depression: Another major trial (within the VITAL framework) found that Vitamin D3 supplementation in adults did not significantly prevent depression—so this effect is not established for everyone, particularly in those without severe deficiency.
🧠 Multiple Sclerosis (MS): A Two-Layer Picture of Evidence
🧩 In people with MS, a 2024 meta-analysis of RCTs reported that Vitamin D3 supplementation did not show a clear, statistically significant effect on major clinical outcomes—though some imaging markers showed minor favorable trends.
⚡ However, in 2025, an RCT using very high intermittent dosing (100,000 IU every two weeks) in individuals with CIS / early-stage MS showed a reduction in disease activity, suggesting that disease stage, dosing strategy, and patient selection might all be key factors. More confirmation is still needed.
🍬 Type 2 Diabetes: In the D2d trial (participants at high risk for diabetes), Vitamin D3 supplementation did not significantly or conclusively reduce diabetes incidence. Therefore, the claim that “Vitamin D prevents diabetes in everyone” lacks strong evidence.
⚖️ Weight Loss: Meta-analyses generally show that Vitamin D alone does not cause meaningful or sustained reductions in body weight or fat mass. When changes occur, they are usually small and context-dependent—for example, in conjunction with weight-loss programs or among those with deficiency.
🧩 Why Do Study Results Sometimes Conflict?
The Role of Baseline Levels
🧪 One of the main reasons results differ is that many large RCTs were conducted in generally healthy populations, where most participants did not have severe deficiency at baseline—so expecting a “big effect” isn’t realistic.
🎯 When someone truly has a deficiency, the body benefits from correction—but when levels are already sufficient, adding more doesn’t push performance or health several levels higher.
🧫 A second reason is differences in study design: dosing pattern (daily vs. bolus), duration, adherence, methods of measuring 25(OH)D, and what specific outcomes the trial was designed to test.
🧠 Professional takeaway for readers: Think of Vitamin D as a tool to correct deficiency and support skeletal health. For many of the “big claims” (heart, cancer, mood, weight), if you’re not deficient, expecting a miracle isn’t aligned with scientific reality.
Side Effects, Toxicity, and Red Flags of Vitamin D
🛑 What Is Vitamin D Toxicity and How Does It Happen?
Mostly from Excess Supplements
💊 Vitamin D toxicity occurs when intake becomes so excessive—usually from high-dose supplements or pharmaceutical preparations—that it leads to abnormally high calcium levels in the body, causing systemic effects.
🧯 Toxicity is almost always the result of supplement overuse (or accidental overlap of multiple high-dose products), not from ordinary food sources.
⚠️ Combining high Vitamin D intake with calcium supplements, especially when done without clear need or for extended periods, can increase the risk of complications and must be managed carefully.

🧠 Main Mechanism: Why Too Much Becomes Dangerous
What We Know / What We Don’t
🧬 When Vitamin D levels rise excessively, its calcium-regulating effects become amplified, leading to increased calcium absorption in the intestines, and eventually hypercalcemia (high blood calcium) and hypercalciuria (high urinary calcium).
🪨 These imbalances can cause kidney stones, calcium deposits in the kidneys (nephrocalcinosis), reduced kidney function, and in severe cases, cardiac disturbances or soft-tissue calcification.
🚨 Key Symptoms
When to Take It Seriously
🤢 Early symptoms are often digestive, including loss of appetite, nausea, vomiting, constipation, or abdominal pain.
🚰 Classic signs of hypercalcemia also affect the kidneys and hydration, such as excessive thirst, frequent urination, dehydration, weakness, and fatigue.
🧠 In more severe cases, neurological symptoms may appear—such as confusion, poor concentration, drowsiness, and in acute situations, even emergency-level conditions.
🪨 If you have a history of kidney stones, or suddenly experience flank pain, painful urination, or signs of stones while taking high doses of Vitamin D (or D + calcium), the issue should be taken seriously and medically evaluated.
🌞 Why You Can’t Get “Toxic” from Sunlight
The Body Has a Built-In Limit
☀️ The body has a natural braking mechanism for Vitamin D synthesis in the skin: with continued sun exposure, precursors and intermediates are photoconverted into other compounds, preventing endless Vitamin D production.
🧴 Therefore, Vitamin D toxicity doesn’t come from sunlight; the real risk usually comes from excessive supplement use or stacking multiple Vitamin D–containing products at once.
⛔ Common Red Lines
Mistakes That Cause the Most Harm
📦 Taking multiple products that each contain Vitamin D (a multivitamin + standalone D + bone/calcium supplement, etc.) without adding up the total dose.
📅 Using high doses for long periods under the assumption that “more is better,” when in reality, Vitamin D has a safety ceiling.
💉 Self-injecting or taking high-dose bolus formulations without a clear medical reason and without proper lab monitoring.
🧪 Treating deficiency with large doses without tracking 25(OH)D, calcium, and when relevant, kidney function, can lead to preventable complications.
🧷 Who Should Be Extra Cautious?
🪨 People with a history or risk of kidney stones, especially those taking calcium supplements simultaneously, should follow a more cautious and well-monitored plan.
🩺 Individuals with kidney disease or disorders involving calcium or the parathyroid glands, since their calcium regulation and tolerance may be more sensitive.
🧫 Those with granulomatous diseases (like sarcoidosis or certain infections such as tuberculosis) or some lymphomas, as they may produce extra 1,25(OH)₂D outside the kidneys, making them prone to hypercalcemia even at normal doses.
💊 People taking medications that affect calcium or kidney function (e.g., thiazide diuretics in certain cases) should have personalized supplementation plans.
🍼 Infants and young children are particularly sensitive to dosing and should receive supplements only according to standard recommendations, with careful attention to drop count and units.
✅ Safe and Practical Summary
🧭 If your goal is maintenance, there’s no need to approach high doses; the aim is to achieve adequate and stable intake.
🧪 If you’re aiming to correct a deficiency or using higher doses, the best approach is a targeted plan with periodic monitoring of 25(OH)D (and calcium/kidney function if necessary).
🚑 If you experience symptoms of hypercalcemia or have taken very high doses, treat it as a medical issue that requires prompt evaluation.
Drug Interactions and Contraindications / Cautions for Vitamin D
🧠 Vitamin D may seem “simple,” but because it affects the calcium–phosphate axis and involves complex absorption and metabolism pathways, certain medications can:
🧩 Reduce its absorption
🧩 Lower its blood levels
🧩 Or increase the risk of hypercalcemia or kidney stones when combined with high doses.
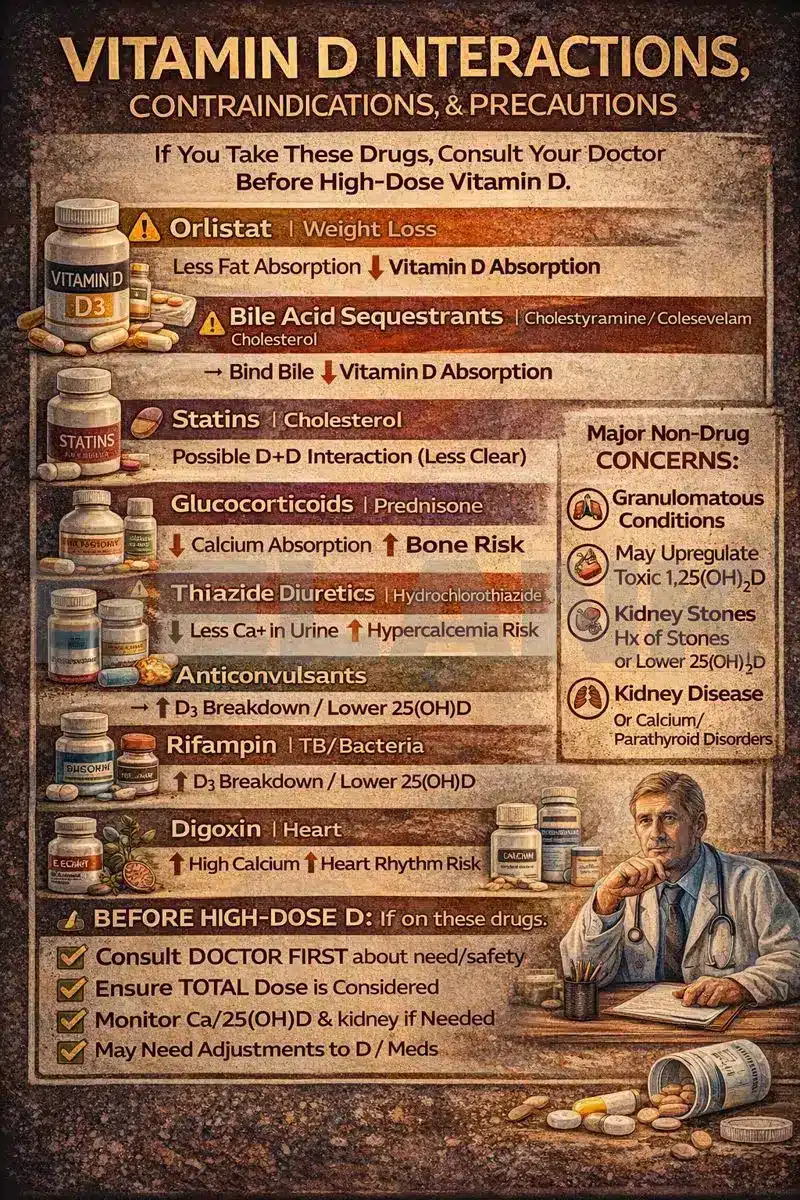
💊 List of Important Drugs
And the Specific Issues They Cause
🟠 1) Orlistat
What It Does
🧴 Orlistat reduces fat absorption; since Vitamin D is fat-soluble, its absorption may decrease, leading to lower 25(OH)D levels.
✅ Practical tip: If you take Orlistat, fat-soluble vitamins (A, D, E, K) should be taken at a different time of day, and periodic monitoring may be needed.
🟡 2) Bile Acid Sequestrants
Examples: Cholestyramine / Colestipol / Colesevelam
🧲 These drugs can reduce the absorption of fats and fat-soluble vitamins, meaning normal dietary Vitamin D intake may no longer be sufficient.
✅ Practical tip: Take Vitamin D at a different time from these drugs and consider monitoring Vitamin D levels if you’re in a high-risk group.
🟣 3) Statins
Potential Two-Way Interaction
🧾 Regarding statins, there’s no strong or definitive interaction like that seen with Orlistat. However, official sources list statins among the drugs that may interact with Vitamin D or require attention in certain situations.
✅ Practical tip: If you’re taking a statin, standard Vitamin D doses are generally safe. Avoid starting high doses unnecessarily, and if you’re also taking other supplements, always consider the total Vitamin D amount and your kidney/calcium status.
🔴 4) Glucocorticoids (Steroids)
Example: Prednisone
🩺 Long-term corticosteroid use can reduce calcium absorption, alter bone metabolism, and affect Vitamin D activity, thereby increasing the risk of bone loss or osteoporosis.
✅ Practical tip: During chronic steroid therapy, Vitamin D becomes part of a broader bone health strategy, and targeted monitoring and supplementation are often recommended.
🟤 5) Thiazide Diuretics
Example: Hydrochlorothiazide
💧 Thiazides reduce calcium excretion in urine; in some individuals, the combination of thiazides + high Vitamin D doses can increase the risk of hypercalcemia.
⚠️ Practical tip: If you’re taking a thiazide diuretic—especially when using higher-than-maintenance doses of Vitamin D—it’s best to coordinate with your doctor for monitoring.
🟢 6) Anticonvulsants (Certain Anti-Seizure Drugs)
Examples: Phenytoin / Phenobarbital / Carbamazepine
⚙️ Some anticonvulsants accelerate Vitamin D metabolism, which can lower 25(OH)D levels or cause them to drop faster over time.
✅ Practical tip: For patients on long-term anticonvulsants, personalized monitoring and dosing adjustments are especially important.
🟦 7) Rifampin (and Similar Enzyme Inducers)
Examples: Rifampin and related enzyme inducers
🧬 These drugs can increase Vitamin D breakdown in the liver, leading to lower blood levels of 25(OH)D.
✅ Practical tip: During long-term Rifampin therapy, periodic monitoring and management of 25(OH)D levels may be necessary.
🟫 8) Digoxin
and Similar Cardiac Glycosides
❤️ If Vitamin D overdose leads to hypercalcemia, it can increase the risk of cardiac arrhythmias in people taking digoxin.
🚫 Practical tip: In this group, high-dose Vitamin D should never be used without medical supervision.
🧊 9) Aluminum-Containing Antacids
(Aluminum-Based Antacids) in Kidney Disease
🩺 In some patients with chronic kidney disease, long-term aluminum exposure combined with altered calcium/Vitamin D metabolism can become problematic.
✅ Practical tip: This concern mainly applies to specific clinical settings under medical supervision.
⛔ Major Contraindications / Cautions
Non-Drug but Critical Conditions
🧫 Granulomatous diseases (e.g., sarcoidosis) and certain lymphomas: the body may overproduce 1,25(OH)₂D beyond normal regulation, leading to hypercalcemia even with standard doses.
🪨 History of kidney stones or hypercalciuria, especially when combined with calcium supplements.
🩺 Kidney disease or parathyroid/calcium disorders: any high-dose plan must be targeted and closely monitored.
✅ Quick Checklist
✅ If you take any of these medications, consult your doctor before starting high-dose Vitamin D.
📌 If any of the following apply to you, consult your doctor before using high doses (e.g., near the UL or therapeutic levels):
🟠 You’re taking Orlistat or other fat absorption–blocking drugs.
🟡 You’re on bile acid sequestrants (e.g., Cholestyramine / Colesevelam / Colestipol).
🟢 You use anti-seizure medications (phenytoin / phenobarbital / carbamazepine).
🔴 You’re on long-term oral corticosteroids (e.g., prednisone or similar).
🟤 You take thiazide diuretics (e.g., hydrochlorothiazide or similar).
🟦 You use Rifampin or other liver enzyme–inducing drugs.
🟫 You take Digoxin.
🪨 You have a history of kidney stones or hypercalciuria, or you’re taking calcium supplements simultaneously.
🩺 You have kidney disease, sarcoidosis, or parathyroid/calcium metabolism disorders.
✅ Practical takeaway: In these cases, the issue isn’t just “Vitamin D”—it’s the entire calcium–kidney–medication axis. The right decision means a rational dose + follow-up testing when necessary.
Vitamin D Label Reading in the United States
IU, mcg, and Daily Value
🧾 In the U.S. market, if you know how to read the label correctly, 80% of common mistakes (wrong dosage, poor product choice, double-dosing with a multivitamin) are solved right there—so treat this section as an “essential skill.”
🔁 IU ↔ mcg Conversion (Fixed Rule)
And what problems they actually cause
🧮 The vitamin D conversion rule is fixed: 1 mcg = 40 IU (and conversely, 1 IU = 0.025 mcg).
✅ This means: no matter how the amount is shown on the label, you can convert it quickly.
🧠 A few golden conversions you’ll always need:
🔹 10 mcg = 400 IU
🔹 15 mcg = 600 IU
🔹 20 mcg = 800 IU
🔹 50 mcg = 2000 IU
🔹 100 mcg = 4000 IU
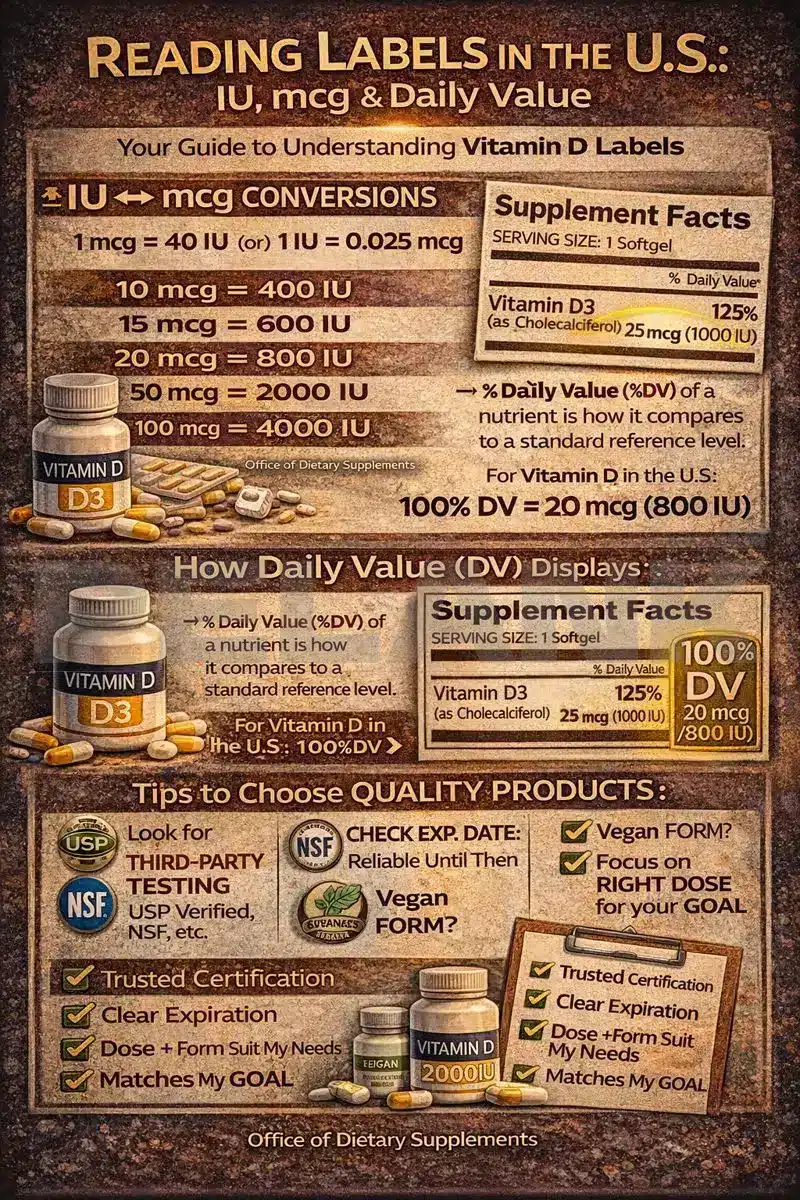
🏷️ What does vitamin D DV mean in the U.S., and how is it shown on the label?
And what problems they actually cause
🇺🇸 On U.S. labels, you usually see two things:
✅ The amount of vitamin D (for example, 20 mcg or 800 IU)
✅ %DV, meaning the percentage of the “Daily Value”
📌 Vitamin D DV in the U.S. = 20 mcg per day (equivalent to 800 IU), and %DV is calculated based on this value.
🧾 So if you see this on a supplement:
🟢 Vitamin D 20 mcg (800 IU) — 100% DV
it means that product provides exactly the U.S. daily DV and covers 100% of it.
🔍 Practical tip:
🧠 DV is a “label reference number,” not a medical prescription; this means some people (such as older adults, high-risk individuals, or those correcting a deficiency) may need a different dose, but DV helps you compare products quickly and consistently.
🧾 What exactly should we look for on the Supplement Facts label?
🔎 When you check the Supplement Facts panel, run through this checklist:
✅ 1) Find the form:
🧬 See whether it says Vitamin D3 (Cholecalciferol) or Vitamin D2 (Ergocalciferol).
✅ 2) Read the actual amount with the correct unit:
🧮 In the U.S., it’s usually listed in mcg, and IU is often shown in parentheses as well.
✅ 3) Check the servings:
🍽️ If it says “Serving Size: 2 softgels,” the amount you see is for 2 capsules, not 1.
✅ 4) Avoid double-dosing:
📦 Many people take a multivitamin + a separate Vitamin D supplement + a bone product at the same time, and the total dose climbs without them realizing it; this is exactly where label reading prevents mistakes.
🛡️ How can we choose a higher-quality product?
🧪 The reality of the supplement market is that “not all products are created equal,” so smart selection means focusing on quality control and transparency.
🏅 1) Third-party testing (the best purchase filter)
✅ If you see that a product or its official website shows testing by a reputable third party, the risk of label inaccuracies or contamination is lower.
🔹 USP Verified (confirms the product contains what the label claims and is manufactured to quality standards)
🔹 NSF Certified for Sport (especially important for athletes: screening for banned substances and stricter quality control)
🧠 Important note: don’t rely solely on a brand’s claim of “third-party tested”; the seal or program name should be real and verifiable.
📅 2) Expiration date and storage conditions
⏳ Vitamin D is relatively stable, but packaging quality, heat/light exposure, and the expiration date affect how much you can trust the actual dose until the end of its shelf life.
🌱 3) Vegan form (if it matters to you)
🍃 If you’re vegan, look for Vegan D3 (lichen); just because it’s D3 doesn’t automatically mean it’s animal-derived—vegan versions are now widely available.
🎯 4) The actual dose should align with your goal
🧭 If your goal is maintenance or meeting adequate intake, very high doses are usually not a smart choice.
⚠️ If the goal is “correcting a deficiency,” dosing decisions are better made alongside testing and monitoring (not just buying a 10,000 IU product because it’s “stronger”).
🏃♂️ 5) One extra point for athletes
🧪 If you’re an athlete, prioritize products that are genuinely certified by a recognized program like NSF Certified for Sport, to reduce the risk of contamination with banned substances.
Differences in recommendations across organizations and countries
IU, mcg, and Daily Value
🧩 Why aren’t the guidelines the same?
The roots of the differences
🎯 Each guideline is written for a specific “goal”: some focus on disease prevention in healthy individuals, while others focus on treating deficiency or managing high-risk patients. This difference in purpose leads to different recommendations.
🧪 The level of evidence strictness also differs: an organization like USPSTF typically relies more on large RCTs and hard outcomes (such as fractures or falls) for public recommendations; if a clear benefit isn’t shown, the guidance becomes more conservative.
👥 The “target population” matters: results seen in generally healthy people with average baseline levels may differ from outcomes in deficient individuals, older adults, those with malabsorption, or institutionalized populations.
🌍 Countries also differ in context: food fortification policies, sunlight exposure, lifestyle, and even public health strategies all influence the population’s “true needs,” and therefore the recommendations.
🧠 Endocrine Society (2024 update): the main message for most healthy adults
And the Specific Issues They Cause
✅ In the 2024 guideline (focused on “disease prevention”), the key message is that healthy adults under 75 generally do not show reliable benefit from vitamin D intakes above the RDA/IOM, and typically do not need “doses higher than the reference recommendations.”
🧪 The guideline also states that, due to a lack of sufficient supporting evidence, routine 25(OH)D testing is generally not recommended for individuals without a clear indication.
🟢 Instead, the guideline considers “empiric supplementation” more defensible for certain groups (such as ages 1–18, adults over 75, pregnancy, and some specific groups like high-risk prediabetes).
🧾 USPSTF: avoiding misinterpretation
Screening vs. fall/fracture prevention
🧪 Screening for deficiency in asymptomatic individuals: USPSTF states that for vitamin D deficiency testing/screening in asymptomatic adults, there is insufficient evidence to recommend universal screening (meaning “neither a general endorsement nor a definitive rejection”—but rather “we don’t have enough data for a population-wide recommendation”).
🦴 Prevention of fractures/falls with supplementation in community-dwelling adults: In its December 2024 draft, USPSTF reported that in community-dwelling adults, vitamin D supplementation (with or without calcium) has not shown benefit for primary prevention of fractures, and vitamin D use for fall prevention is also not recommended for specific groups. Important note: these recommendations apply to “primary prevention in the general population,” not to people with diagnosed deficiency, osteoporosis, or clear medical indications.
🔄 NASEM and the future of DRIs
📌 Because nutrition standards may be revised as new evidence emerges, the National Academies (NASEM) continuously monitors updates to the Dietary Reference Intakes (DRIs) for vitamin D and calcium. For this reason, this guide will also be updated if official revisions are released, so it remains current and reliable.
Frequently Asked Questions
FAQ
🧪 If you have clear skeletal or muscular symptoms (bone pain, muscle weakness, low-impact fractures) or are high-risk (severe lack of sun exposure, malabsorption, bariatric surgery, obesity, certain medications), a 25(OH)D test can help guide dosing and duration decisions.
🧭 If you are healthy and low-risk with no specific symptoms, routine universal screening is not definitively recommended, and decisions are better made in a targeted, individualized way.
🧬 For assessing overall vitamin D status, the best and most commonly used marker is 25(OH)D.
⚗️ 1,25(OH)₂D is the active hormonal form and may be normal or even elevated despite deficiency; therefore, it is usually not suitable for screening overall vitamin D status.
📏 The cutoffs vary slightly between organizations.
🧩 Practical takeaway: levels below 20 ng/mL are generally considered deficient/insufficient; above that, they may be considered “adequate” depending on the framework, and at very high levels (for example, above 50 ng/mL), safety concerns arise.
🧠 More important than a single number: individual risk, symptoms, and trends over time.
🧮 Fixed rule: nmol/L = ng/mL × 2.5
🔁 Examples: 20 ng/mL = 50 nmol/L | 30 ng/mL = 75 nmol/L | 50 ng/mL = 125 nmol/L
🏷️ Both are dose units.
🧮 The fixed, global vitamin D conversion: 1 mcg = 40 IU and 1 IU = 0.025 mcg.
📌 The U.S. DV for vitamin D on labels is usually based on 20 mcg (800 IU). Time of day doesn’t matter much; consistency is more important. It’s best taken with a meal that contains some fat to improve absorption.
🟡 Both raise levels, but overall the evidence suggests that D3 generally increases 25(OH)D levels more and maintains them more consistently than D2.
🧠 Practical choice for most people: D3 (unless a doctor specifically prescribes D2 or your vegan/access needs are different).
⚡ Calcifediol is 25(OH)D itself (one step ahead of D3/D2).
🚀 Because it bypasses the liver step, it can usually raise blood levels more quickly and sometimes achieve a greater effect with a lower dose.
🧑⚕️ Because of its higher potency and faster action, it’s usually an option best chosen with a physician’s guidance.
🥑 It’s best taken with a meal (preferably one that contains some fat), since it’s fat-soluble and absorption is usually better.
🍽️ If you take it on an empty stomach and don’t see results or experience fluctuations, move it to a main meal.
🕘 There’s no definitive evidence for a single “golden time” that works for everyone; consistency is the most important factor.
🌙 If you feel your sleep quality worsens when taking it at night, the simplest fix is to switch to morning or midday and stick with that timing.
⏳ Levels typically increase over several weeks to a few months, depending on dose, baseline level, body weight, absorption, and adherence.
🧪 If you’ve started a deficiency-correction plan, repeating the test after a reasonable interval (often several weeks to a few months) helps adjust the dose and prevents overshooting.
📅 Daily dosing usually provides more stable levels and is easier for many people.
🗓️ Weekly dosing can be helpful for those who struggle with daily adherence.
🚫 Very large, infrequent “bolus doses” (especially without a clear indication and in older adults) are not a first-choice option, because they cause large fluctuations and have been associated with adverse outcomes in some data.
☀️ Usually no; the body has built-in limiting mechanisms for skin production.
💊 Toxicity almost always comes from excessive supplementation or combining multiple vitamin D–containing products, not from sunlight or normal foods.
🧨 Main mechanism: excessive calcium levels (hypercalcemia/hypercalciuria).
🚨 Key symptoms: nausea/vomiting, constipation, loss of appetite, thirst and frequent urination, weakness, confusion; and in some cases, increased risk of kidney stones and kidney damage.
🛑 If you’ve been taking high doses and have these symptoms, this is a medical issue.
🪨 Vitamin D itself, at reasonable doses, is usually not a problem, but high doses (especially when combined with calcium supplements) can increase risk in some individuals.
🧩 If you have a history of kidney stones, decisions about higher doses should be targeted and cautious.
⚠️ People with a history of kidney stones/hypercalciuria, kidney disease, sarcoidosis/granulomatous diseases, certain lymphomas, or those taking calcium-sensitizing medications (such as thiazides or digoxin).
🧑⚕️ In these groups, “high doses” are not recommended without medical supervision.
📦 First, calculate the total dose: multivitamin + separate vitamin D + bone/calcium products.
🧠 Many people unintentionally end up “double-dosing.” If your multivitamin already gets you to an adequate intake, you may not need separate vitamin D unless you’re high-risk or deficient.
🏋️♂️ If you’re deficient, correcting the deficiency can help muscle function and overall recovery.
🧠 But if your levels are adequate, the evidence does not strongly support “high doses for super-performance.”
📌 For indoor or winter-season athletes, focusing on adequacy (not excess) is more reasonable.
👶 Infants and children need adequate intake for bone growth, and doses should be precise and standardized (especially with liquid drops).
🧠 For these groups, the main goal is usually “meeting the recommended intake,” not high dosing.
🤰 During pregnancy and breastfeeding, adequate intake is important; however, universal screening for all low-risk individuals is not definitively recommended.
🧩 Decisions are best based on risk factors (low sun exposure, diet, prior deficiency, medical conditions) and a clinician’s advice.
🦴 Calcium and vitamin D have a clear relationship (especially for bone health), but calcium supplements are not necessary for everyone.
⚙️ Magnesium is biologically important; if you’re deficient or have low intake, correcting it makes sense—but it’s not a universal rule.
🧡 Regarding K2: the evidence for “universally requiring K2 alongside vitamin D” is not definitive; and if you take warfarin or other anticoagulants, K2 can be sensitive.
Scientific Sources & References
References 📚
[S1] National Institutes of Health, Office of Dietary Supplements. (n.d.). Vitamin D: Fact sheet for health professionals. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
[S2] National Academies of Sciences, Engineering, and Medicine. (2010). Dietary Reference Intakes for Calcium and Vitamin D: Report brief (PDF). https://nap.nationalacademies.org/resource/13050/Vitamin-D-and-Calcium-2010-Report-Brief.pdf
[S3] U.S. Preventive Services Task Force. (2021). Vitamin D deficiency in adults: Screening (Recommendation statement). https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/vitamin-d-deficiency-screening
[S4] Bikle, D. D. (n.d.). Vitamin D: Production, metabolism, and mechanism of action. In Endotext (NCBI Bookshelf). https://www.ncbi.nlm.nih.gov/books/NBK278935/
[S5] Tripkovic, L., et al. (2012). Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: A systematic review and meta-analysis. The American Journal of Clinical Nutrition. https://pubmed.ncbi.nlm.nih.gov/22552031/
[S6] Merck Manual Professional Edition. (n.d.). Hypercalcemia (includes granulomatous disorders & unregulated 1,25(OH)2D conversion). https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/electrolyte-disorders/hypercalcemia
[S7] Wallace, R. B., et al. (2011). Urinary tract stone occurrence in the Women’s Health Initiative randomized clinical trial of calcium and vitamin D supplements. The American Journal of Clinical Nutrition. https://pmc.ncbi.nlm.nih.gov/articles/PMC3127502/
[S8] National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). (n.d.). Calcium and vitamin D: Important for bone health. https://www.niams.nih.gov/health-topics/calcium-and-vitamin-d-important-bone-health
[S9] Manson, J. E., et al. (2019). Vitamin D supplements and prevention of cancer and cardiovascular disease (VITAL). The New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMoa1809944
[S10] Jolliffe, D. A., et al. (2025). Vitamin D supplementation to prevent acute respiratory infections: Systematic review and meta-analysis of stratified aggregate data. The Lancet Diabetes & Endocrinology, 13(4), 307–320. https://www.thelancet.com/journals/landia/article/PIIS2213-8587%2824%2900348-6/fulltext
(A more accessible alternative: https://pubmed.ncbi.nlm.nih.gov/39993397/)
[S11] National Academies of Sciences, Engineering, and Medicine. (n.d.). Dietary Reference Intakes for Calcium and Vitamin D (Chapter 2: serum 25(OH)D thresholds). https://www.nationalacademies.org/read/13050/chapter/2
[S12] Centers for Disease Control and Prevention. (n.d.). Vitamin D Standardization-Certification Program (VDSCP). https://www.cdc.gov/clinical-standardization-programs/php/vitamin-d/index.html
[S13] Holick, M. F., et al. (2011). Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 96(7), 1911–1930. https://academic.oup.com/jcem/article/96/7/1911/2833671
[S14] Endocrine Society. (2024). Vitamin D for the prevention of disease (Guideline resources). https://www.endocrine.org/clinical-practice-guidelines/vitamin-d-for-prevention-of-disease
[S15] American Academy of Pediatrics. (n.d.). Vitamin D for babies, children & adolescents. HealthyChildren.org. https://www.healthychildren.org/English/healthy-living/nutrition/Pages/vitamin-d-on-the-double.aspx
[S16] American College of Obstetricians and Gynecologists. (n.d.). Healthy eating during pregnancy (FAQ). https://www.acog.org/womens-health/faqs/healthy-eating-during-pregnancy
[S17] American College of Obstetricians and Gynecologists. (2011). Vitamin D: Screening and supplementation during pregnancy (Committee Opinion). https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2011/07/vitamin-d-screening-and-supplementation-during-pregnancy
[S18] Sanders, K. M., et al. (2010). Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial. JAMA. https://jamanetwork.com/journals/jama/fullarticle/185854
[S20] Pittas, A. G., et al. (2019). Vitamin D supplementation and prevention of type 2 diabetes (D2d). The New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMoa1900906
[S23] Mahler, J. V., et al. (2024). Vitamin D3 as an add-on treatment for multiple sclerosis: A systematic review and meta-analysis of RCTs. https://pubmed.ncbi.nlm.nih.gov/38211504/
[S24] Thouvenot, E., et al. (2025). High-dose vitamin D in clinically isolated syndrome and early MS (D-Lay MS RCT). JAMA. https://jamanetwork.com/journals/jama/fullarticle/2831270
[S25] Okereke, O. I., et al. (2020). Effect of long-term vitamin D3 supplementation vs placebo on depression risk and mood scores. JAMA. https://jamanetwork.com/journals/jama/fullarticle/2768978
[S26] Merck Manual Professional Edition. (n.d.). Vitamin D toxicity. https://www.merckmanuals.com/professional/nutritional-disorders/vitamin-deficiency-dependency-and-toxicity/vitamin-d-toxicity
[S27] Tebben, P. J., Singh, R. J., & Kumar, R. (2016). Vitamin D-mediated hypercalcemia: Mechanisms, diagnosis, and treatment. Endocrine Reviews. https://pubmed.ncbi.nlm.nih.gov/27588937/
[S28] Bikle, D. D. (n.d.). Vitamin D: Production, metabolism and mechanisms of action (PDF). Endotext. https://www.endotext.org/wp-content/uploads/pdfs/vitamin-d-production-metabolism-and-mechanisms-of-action.pdf
[S29] Endotext (NCBI Bookshelf). (n.d.). Approach to hypercalcemia. https://www.ncbi.nlm.nih.gov/books/NBK279129/
[S30] MedlinePlus. (n.d.). Vitamin D (interactions & precautions). https://medlineplus.gov/vitamind.html
[S31] Cleveland Clinic. (n.d.). Vitamin D deficiency: Causes, symptoms & treatment. https://my.clevelandclinic.org/health/diseases/15050-vitamin-d-vitamin-d-deficiency
[S32] U.S. Pharmacopeia (USP). (n.d.). Dietary Supplement Verification Program. https://www.usp.org/verification-services/dietary-supplements-verification-program
[S33] NSF. (n.d.). Certified for Sport®. https://www.nsfsport.com/
[S34] Operation Supplement Safety (OPSS). (n.d.). Why is third-party certification important for dietary supplements? https://www.opss.org/article/why-third-party-certification-important-dietary-supplements
[S35] NIH, Dietary Supplement Ingredient Database (DSID). (n.d.). Unit conversions (Vitamin D: IU ↔ mcg). https://dsid.od.nih.gov/Conversions.php
[S36] U.S. Preventive Services Task Force. (2024, December 17). Draft recommendation: Vitamin D, calcium, or combined supplementation for the primary prevention of falls and fractures in community-dwelling adults. https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/vitamin-d-calcium-combined-supplementation-primary-prevention-falls-fractures-communitydwelling-adults
[S37] Endocrine Society. (2024). Guideline recommends healthy adults under 75 take the recommended daily allowance of vitamin D (News release). https://www.endocrine.org/news-and-advocacy/news-room/2024/endocrine-society-recommends-healthy-adults-take-the-recommended-daily-allowance-of-vitamin-d
[S38] National Academies of Sciences, Engineering, and Medicine. (n.d.). Dietary Reference Intakes for Calcium and Vitamin D (project page / update effort). https://www.nationalacademies.org/projects/FNBX-H-08-08-A/publication/13050
Pelank Life | Body Health Assessment
The Best Body Health Calculators Using Scientific Methods
Developed by Pelank Life ©

Mohsen Taheri
December 23, 2025