Attention Deficit or Hyperactivity Disorder (ADHD)
ADHD (Attention-Deficit/Hyperactivity Disorder)
Attention-Deficit/Hyperactivity Disorder (ADHD) is one of the most well-known and yet complex psychiatric disorders that affects a wide range of children and adults around the world. This disorder is characterized by three main features: inattention, hyperactivity, and impulsivity. However, the reality goes beyond these labels.
In many societies, ADHD is still associated with misunderstandings and misconceptions. Individuals affected, especially during childhood, may be labeled as “lazy,” “disorganized,” or “overactive,” while the core issue stems from structural and chemical differences in the brain. Therefore, accurate and scientific awareness about this disorder is of vital importance.
🔍 Prevalence of ADHD Worldwide
According to reliable global statistics:
Approximately 5 to 7 percent of school-age children are affected by ADHD.
Around 60% of these children carry persistent symptoms into adulthood.
The prevalence in adults is estimated to be around 2.5 to 3 percent.
Although it is commonly believed that ADHD only occurs in children, the reality is that this disorder not only persists into adulthood but, without diagnosis and treatment, can lead to serious issues in one’s career, relationships, education, and self-esteem.
🎯 What is the purpose of this article?
The purpose of this article is to scientifically, clearly, and systematically explore all aspects of this disorder and answer the following questions:
What exactly is ADHD and how does it manifest?
How can it be diagnosed and treated?
What challenges come with living with ADHD?
What types of support are essential for individuals with ADHD?
What scientific findings and new technologies in 2025 have helped in managing ADHD?
Ultimately, this article aims to take a small but effective step toward supporting individuals with ADHD by reducing stigmatization, increasing understanding, and providing useful tools for better management of the disorder.
What is ADHD?
Scientific Definition / Types of ADHD
ADHD, or Attention-Deficit/Hyperactivity Disorder, is one of the most common neurodevelopmental disorders, primarily diagnosed during childhood but can continue into adulthood. This disorder affects an individual’s ability to focus, their level of physical activity, and their ability to control impulses.
🔬 Scientific Definition of ADHD
According to the definition by the American Psychiatric Association (APA) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), ADHD is a persistent pattern of inattention and/or hyperactivity-impulsivity that is inconsistent with an individual’s developmental level and causes significant impairment in social, academic, or occupational functioning.
This disorder arises due to differences in brain structure, the functioning of neurotransmitters (such as dopamine and norepinephrine), and the development of specific brain regions, such as the frontal lobe.
🧩 Types of ADHD
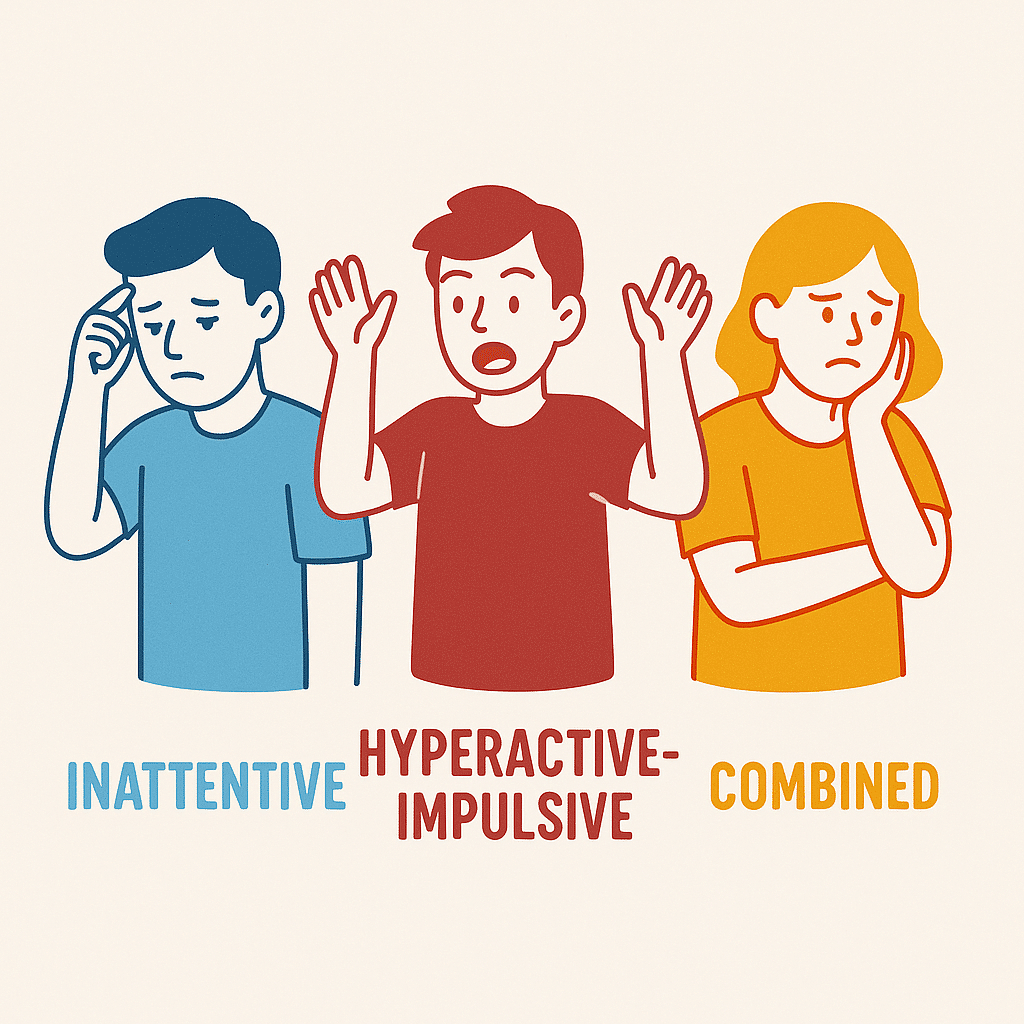
Based on the combination of symptoms, ADHD is divided into three main types:
1. 🟦 Inattentive Type
In this type, symptoms of inattention are predominant, and the individual may:
Fail to pay attention to details or make careless mistakes.
Have difficulty maintaining sustained focus.
Easily get distracted.
Forget to complete tasks or leave them unfinished.
Have difficulty following instructions.
🧩 This type is more commonly seen in girls and adults and may remain undiagnosed for a long time.
2. 🟥 Hyperactive-Impulsive Type
In this type, hyperactivity and impulsivity play the main role:
The individual is constantly on the move (fidgeting, getting up unnecessarily).
Cannot sit still.
Talks excessively or interrupts others during conversations.
Acts or responds without thinking.
Has difficulty waiting their turn.
🧩 This type is more commonly seen in boys at younger ages and is often noticeable in school.
3. 🟨 Combined Type
This type is the most common form of ADHD, combining symptoms of inattention and hyperactivity-impulsivity.
To diagnose this type, the individual must meet the criteria for both categories of symptoms for at least six months.
🔖 Knowing the type of ADHD helps design more tailored treatments and support strategies. Additionally, parents, teachers, and counselors can more purposefully address the individual’s challenges.
Signs and Symptoms of ADHD
Two Groups: Children and Adults
The symptoms of Attention-Deficit/Hyperactivity Disorder (ADHD) are diverse and may appear in various forms depending on age, gender, environment, and the type of ADHD. These symptoms typically begin in childhood and, if untreated, can continue into adulthood. For better understanding, we will separately examine the symptoms in two groups: children and adults:
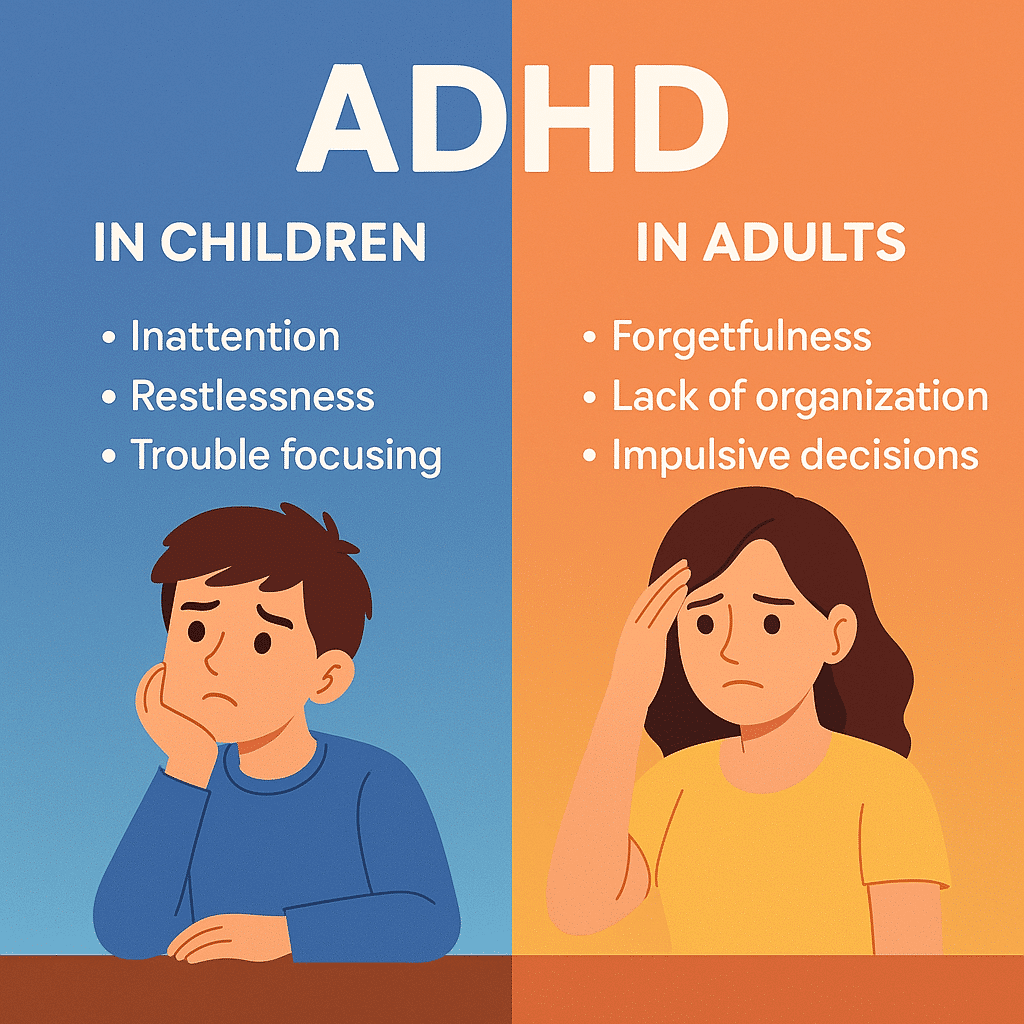
👧🏻🧒🏻 Symptoms of ADHD in Children
In children, ADHD typically manifests more in school, home environments, or social situations. The most important signs include:
🟦 Symptoms of Inattention
Inability to maintain long-term focus on tasks or activities.
Inattention to details and careless mistakes in schoolwork.
Forgetfulness in completing daily tasks (such as bringing books, doing homework).
Incomplete following of instructions.
Losing necessary items such as pencils, toys, or books.
Avoidance of tasks that require sustained concentration.
Easily distracted by even the slightest environmental stimuli.
🟥 Symptoms of Hyperactivity & Impulsivity
Constant restlessness (fidgeting with hands and feet, constant shifting in the seat).
Inability to sit still for long periods (e.g., in class or during meals).
Excessive talking.
Interrupting others during conversations.
Running or climbing on objects in inappropriate situations.
Inability to wait one’s turn.
Impulsive behaviors without considering the consequences.
📌 Important Note: Symptoms must be persistent for at least 6 months and occur in two or more settings (e.g., home and school) to be considered as ADHD.
🧔🏻♀️ Symptoms of ADHD in Adults
The symptoms of ADHD in adulthood are typically more complex and subtle. Many adults with ADHD have been mistakenly labeled for years with terms such as “scatterbrained,” “inability to concentrate,” or even “laziness.” The most common symptoms include:
🟦 Difficulty with focus and inattention
Difficulty prioritizing and managing time.
Frequent forgetfulness of appointments, paying bills, or work tasks.
Starting multiple tasks simultaneously and leaving them unfinished.
The need for external stimuli to focus (e.g., music or time pressure).
🟥 Impulsive behaviors
Impulse purchases followed by regret.
Interrupting others or responding without thinking.
Inability to manage emotions (such as sudden anger or anxiety).
Making quick decisions without considering the consequences.
🟨 Inner and physical restlessness
Feeling the need for constant activity.
Difficulty relaxing or settling down, even in quiet environments.
Experiencing “constant mental pressure” and rapid thoughts.
💔 Social and Occupational Challenges
Difficulty maintaining long-term relationships (due to forgetfulness or impulsive reactions).
Job dissatisfaction due to unfinished projects or frequent procrastination.
Reduced self-esteem due to past failed experiences.
🧭 Gender Differences in Symptoms
In boys, hyperactivity symptoms are more prominent, leading to earlier diagnoses.
In girls, the symptoms are often of the inattentive and more internalized type, which may lead to them being overlooked for years.
⚠️ Why is diagnosis difficult?
ADHD is often mistaken for or overlaps with other disorders, including:
Anxiety disorder
Depressive disorder
Learning disorder
Mild Autism Spectrum Disorder (ASD)
An accurate diagnosis requires a professional psychological evaluation.
Causes and Contributing Factors of ADHD
Genetics / Brain Structure / Environmental Factors
Attention-Deficit/Hyperactivity Disorder (ADHD), contrary to some common beliefs, is not the result of poor upbringing, laziness, or disorganization. This disorder originates from a combination of genetic, biological, and environmental factors. Scientific research in recent decades has shown that ADHD is one of the most influential genetic disorders in psychology, but the role of environmental factors should not be overlooked.
Next, we will discuss the three main causes of this disorder:
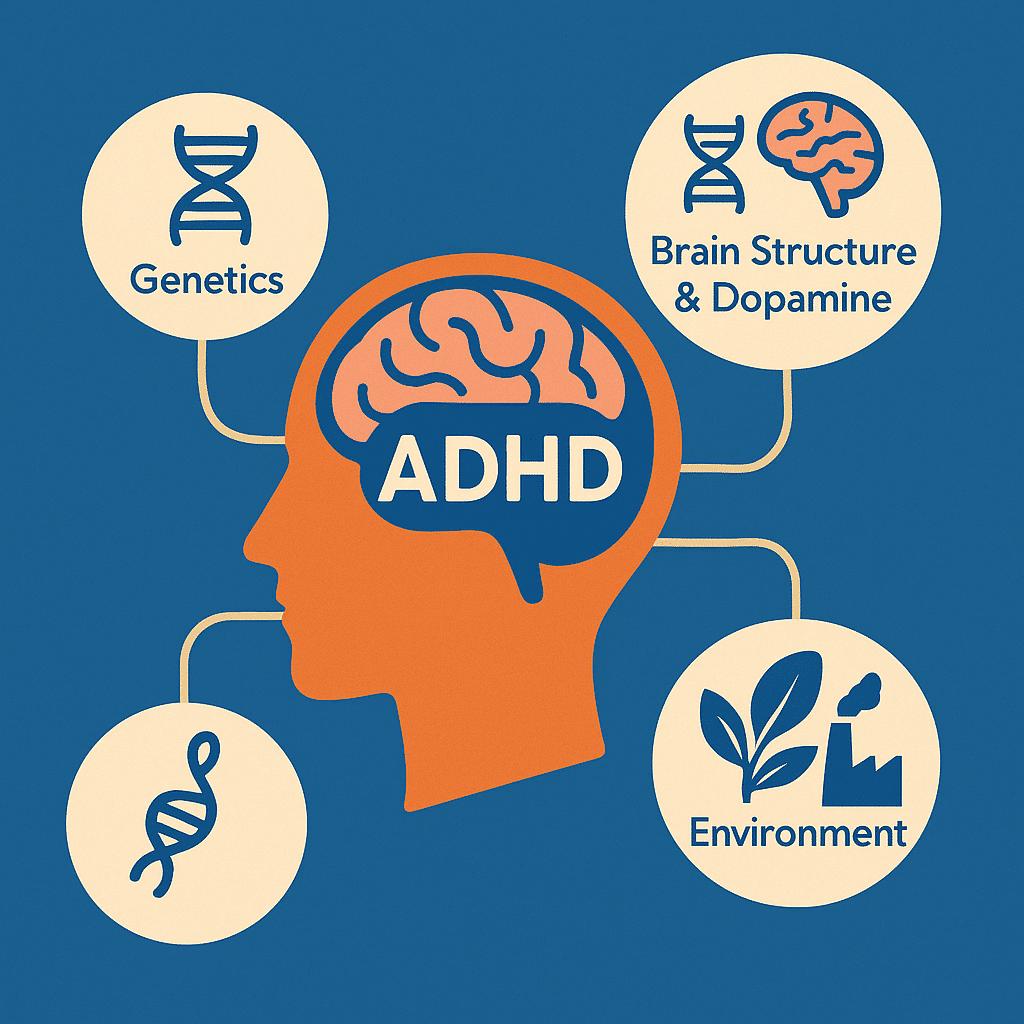
🧬 1. Genetics and Heredity: The Primary Basis for ADHD Development
Studies on twins and families have shown that genetics play a role in 75 to 80 percent of ADHD cases. If one of the parents or siblings of an individual has ADHD, the likelihood of the individual also developing ADHD increases significantly.
Key Points:
ADHD is highly hereditary, and specific genes have been identified as being associated with it (such as genes related to the neurotransmitter dopamine).
In many cases, one or both parents of a child with ADHD may have mild or undiagnosed symptoms of ADHD themselves.
The genetic transmission is usually multifactorial, meaning that several genes work together to influence the development of ADHD, rather than a single specific gene.
📌 Reminder: Genetics provide the predisposition, but the onset or severity of ADHD may be influenced by other factors.
🧠 2. Brain Structure and Neurotransmitter Function
Brain imaging studies (such as fMRI and PET scans) have shown differences in the brains of individuals with ADHD compared to those without the disorder. These differences are observed not only in the brain’s structure but also in its function.
The main differences are:
Decreased activity in the prefrontal cortex: This area is responsible for executive functions such as focus, planning, and impulse control.
Decreased levels of dopamine and norepinephrine: These two neurotransmitters play a crucial role in reward, motivation, attention, and emotional regulation.
Delayed brain maturation: Some areas of the brain in individuals with ADHD develop more slowly than usual, especially in children and adolescents.
🧩 These biological differences are the primary cause of difficulties in focus, behavior control, and restlessness, not a lack of willpower or poor upbringing.
🌍 3. Environmental Factors: A Complementary and Sometimes Triggering Role
In addition to genetic and brain-based factors, certain environmental factors can play a role in the onset or exacerbation of ADHD symptoms:
Before birth (pregnancy):
Maternal smoking or alcohol consumption.
Maternal exposure to severe stress.
Poor nutrition or nutrient deficiencies (such as omega-3 fatty acids or iron).
Exposure to environmental toxins (such as lead).
After birth and in childhood:
Premature birth or low birth weight.
Brain injuries during infancy (such as oxygen deprivation during childbirth).
Exposure to stressful, unstructured, and chaotic environments.
Chronic exposure to excessive light, loud noises, or overuse of digital devices (discussed in some studies but still controversial).
📌 These factors usually do not cause ADHD on their own, but they can trigger or exacerbate symptoms in individuals who are genetically predisposed.
🧭 Summary of This Section:
| Type of factor | Examples | Role |
|---|---|---|
| Genetic | Family history, dopamine-related genes | Primary and determining |
| Biological (Brain-related) | Differences in brain structure and function | Underlying behavioral symptoms |
| Environmental | Stress, nutrition, pre- and post-birth injuries | Triggering or exacerbating factors |
Diagnosis of ADHD |
Tests / Psychologist
Unlike some physical disorders, the diagnosis of ADHD is not based on a blood test or imaging. Instead, it is a multi-step, precise, and clinical process that requires an assessment of behavior, family history, environmental conditions, and alignment with psychiatric criteria.
🧪 Tests and diagnostic tools
There is no specific physical or biological test for the definitive diagnosis of ADHD. However, psychologists and psychiatrists use a range of questionnaires, behavioral assessments, and clinical interviews. The most important tools include:
📝 Standard questionnaires:
Vanderbilt ADHD Diagnostic Rating Scales: A questionnaire for parents and teachers focusing on the core symptoms of ADHD and comorbid disorders.
Conners Rating Scale: One of the most widely used screening tools, completed from the perspective of the parent, teacher, or the individual themselves.
SNAP-IV Questionnaire: Includes 18 key questions based on DSM-5 criteria to assess the three subtypes of ADHD.
📌 These tools are not definitive diagnostic instruments; rather, they are used as part of the preliminary assessment process.
🧠 Role of Psychologist and Psychiatrist in Diagnosis
Accurate diagnosis requires a combination of information from multiple sources. This is where the role of specialists becomes crucial:
👩⚕️ Psychologist:
Conducting cognitive assessments, attention and concentration tests, and evaluating executive skills.
Interviewing parents, teachers, or significant others.
Analyzing reports to understand behavioral patterns.
👨⚕️ Psychiatrist:
Reviewing symptoms alongside medical and family history.
Examining the possibility of comorbid disorders (such as anxiety, depression, autism, sleep disorders).
If necessary, prescribing medication or referring for additional tests.
📌 Sometimes, a definitive diagnosis requires a multi-faceted evaluation in collaboration with a psychiatrist, psychologist, teacher, and parents.
🔎 Differentiating ADHD from other similar disorders
The diagnosis of ADHD has a major challenge: many of its symptoms overlap with other disorders. If misdiagnosed, effective treatment will not occur. Some similar or overlapping disorders include:
| Disorder | Common symptoms with ADHD | Key difference |
|---|---|---|
| Anxiety Disorder | Restlessness, difficulty concentrating | Caused by excessive worry, not an inherent attention problem. |
| Learning Disorder | Academic underachievement, lack of interest in studies | Occurs in one or more specific areas (e.g., reading or mathematics). |
| Autism (ASD) | Attention problems, social interaction difficulties | Repetitive behavioral patterns, difficulty understanding others’ emotions. |
| Depression | Inattention, fatigue, reduced motivation | Often accompanied by sadness, low energy, and isolation. |
| Sleep Disorder | Distraction, irritability | Symptoms improve after sufficient sleep. |
🔔 For this reason, the diagnosis of ADHD must be comprehensive, scientific, and conducted by experienced specialists, not based on superficial observations or simple online tests.
📌 Important note:
Sometimes people think that by simply observing external symptoms like inattention or hyperactivity in a child or themselves, they can diagnose ADHD. However, without thorough evaluation, the likelihood of misdiagnosis and incorrect treatment is very high. Sometimes what appears to be ADHD is actually a response to an unsuitable environment or the experience of emotional trauma.
Methods of Treatment and Management of ADHD
Medication treatment / Non-medication treatments
ADHD is not curable, but it is controllable and manageable. A successful treatment approach typically requires a multidimensional combination of medication, behavioral interventions, educational support, and lifestyle changes. The goal of treatment is to reduce symptoms, improve functioning in daily life, and enhance the individual’s quality of life.
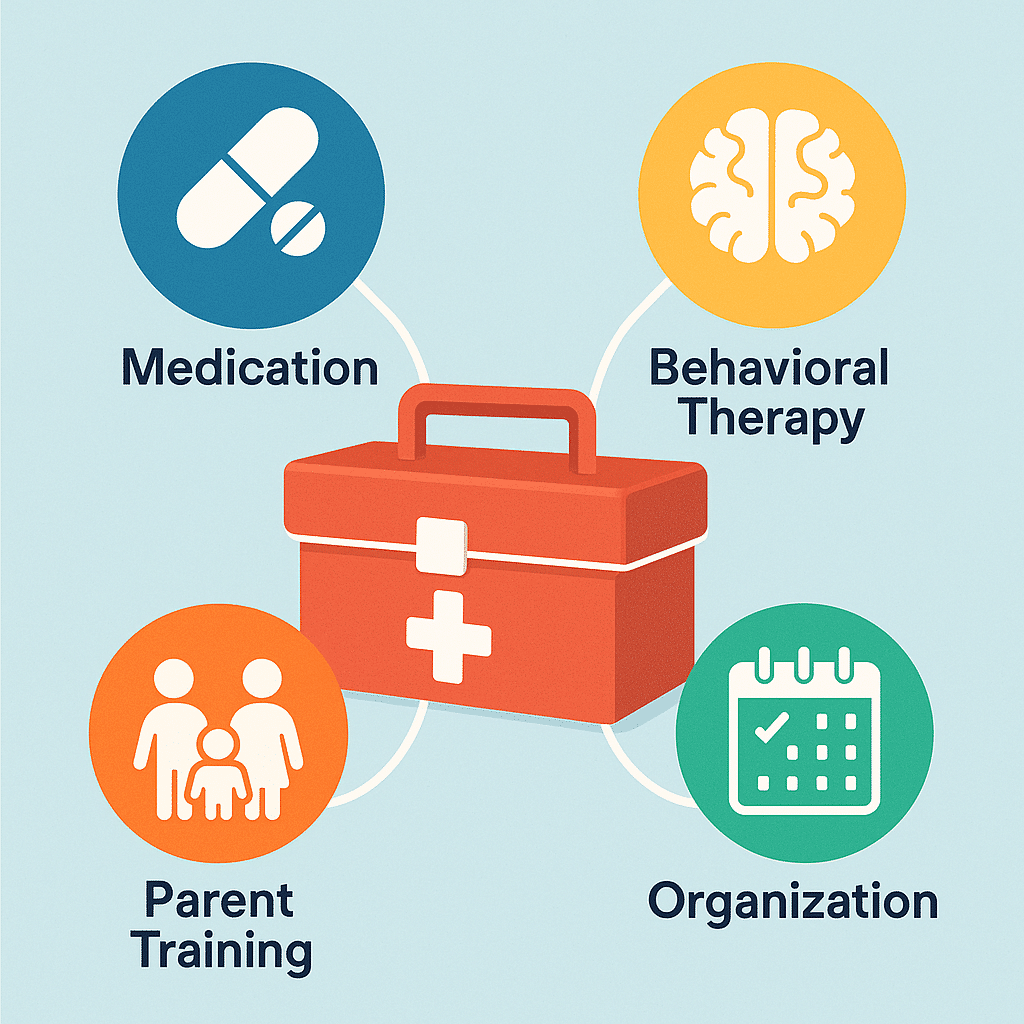
💊 Medication Treatment
Medication treatment is one of the key pillars in managing ADHD, especially in moderate to severe cases.
✅ Stimulant Medications
These are the most common and effective class of medications. They improve concentration, reduce restlessness, and control impulsivity by increasing dopamine and norepinephrine levels in the brain.
Methylphenidate (e.g., Ritalin, Concerta)
Amphetamines (e.g., Adderall, Vyvanse)
📌 The effects of these medications are usually noticeable in a short period, but adjusting the dosage and timing of consumption under medical supervision is essential.
✅ Non-Stimulant Medications
They are used for individuals who do not respond to stimulant medications or experience side effects.
Atomoxetine (Strattera): Norepinephrine enhancer.
Guanfacine and Clonidine: Alpha-2 adrenergic receptor antagonists.
📌 These medications typically take a few weeks to show effects, but they have a longer-lasting impact.
🧠 Non-Medication Treatments
🧩 Cognitive Behavioral Therapy (CBT)
Effective in adolescents and adults for:
Emotion regulation
Increasing self-control
Correcting negative self-beliefs
Improving problem-solving skills
👨👩👧 Parent Training
Parents are taught:
How to reinforce the child’s positive behaviors.
How to appropriately address challenging behaviors.
How to adapt the home environment for a child with ADHD.
🏫 School-based Interventions
Specialized educational programs and teacher support include:
Additional time for exams
Seating the child in a quiet area of the classroom
Providing notes or using audiovisual tools for better comprehension of the lesson.
📅 Practical management and daily strategies
For children and adults, lifestyle management and habit changes play a crucial role in improving performance.
✅ Organizational techniques:
Using a planner, calendar, and reminders.
Creating a daily task list.
Establishing consistent routines.
✅ Lifestyle adjustments:
Regular and sufficient sleep.
Daily physical activity (improving focus and reducing restlessness).
Balanced nutrition, avoiding simple sugars and stimulants.
Limiting the use of digital devices.
✅ Helpful apps:
Apps such as:
Forest (for focus)
Todoist or Trello (for planning)
Headspace (for meditation and mental relaxation)
👪 The Role of Social and Family Support
Acceptance of ADHD—not only by the individual but also by those around them—is essential. Emotional support, understanding differences, and avoiding labeling can significantly reduce the negative impact of the disorder.
🧭 Summary of This Section:
| Approach | Application | Benefits |
|---|---|---|
| Medication | Rapid symptom reduction | Improved focus, reduced impulsivity |
| CBT | Cognitive and behavioral improvement | Emotion regulation, self-awareness |
| Parent Training | Home management | Strengthened parent-child relationship |
| School-based Interventions | Improved learning | Reduced academic pressure |
| Lifestyle Adjustments | Supportive to treatment | No side effects, long-term benefits |
Living with ADHD
Common Challenges / Positive Aspects
Challenges, adaptations, and growth journey with Attention-Deficit/Hyperactivity Disorder (ADHD)
Having ADHD does not mean being incapable—it means living with a different kind of brain. People with ADHD face unique challenges, but they can also thrive in paths that align more naturally with their mental structure.
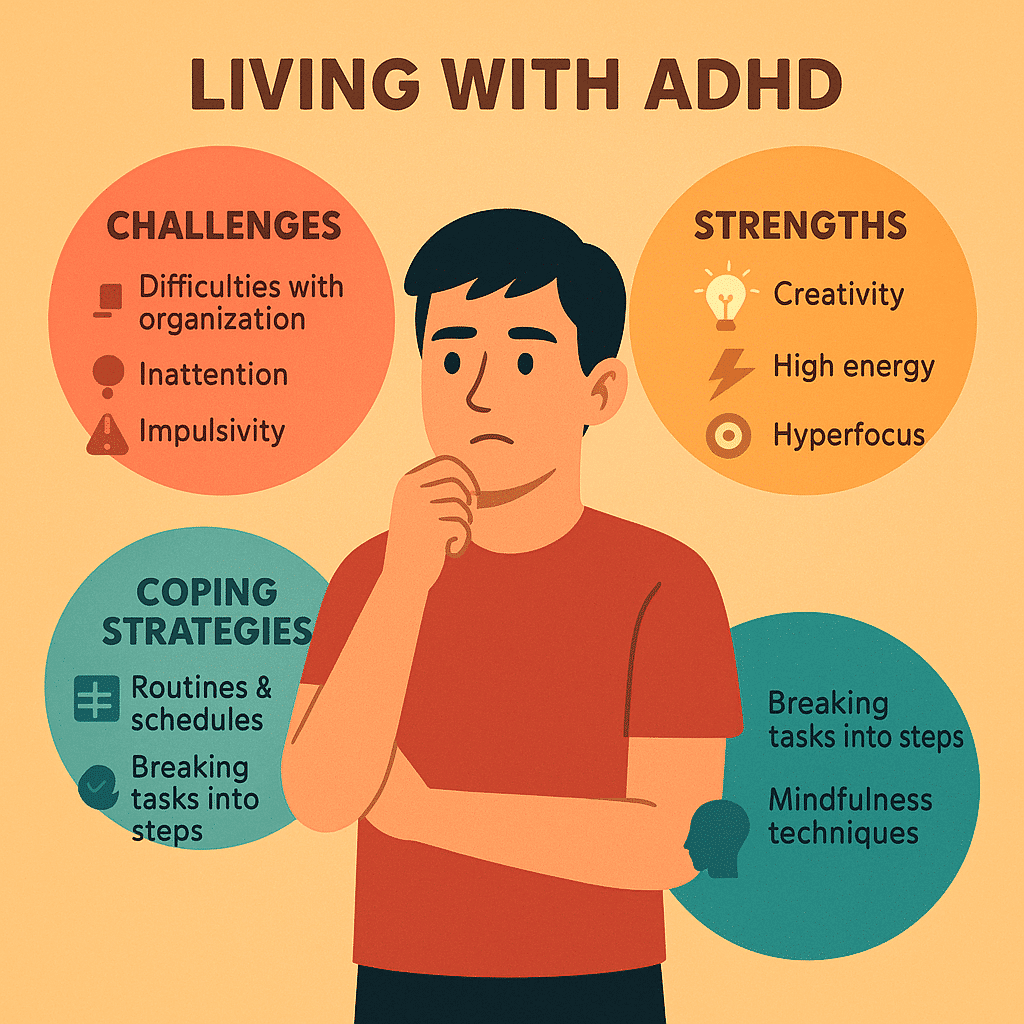
⚠️ Common Challenges in Daily Life
In children:
Academic difficulties: unfinished assignments, difficulty sitting still for long periods in class, inconsistent performance.
Social difficulties: tendency to interrupt others, difficulty taking turns or following game rules.
Low self-esteem: receiving frequent negative feedback from parents, teachers, or peers.
In adults:
Poor time management and planning: frequent delays, forgetting appointments, and leaving tasks unfinished.
Job instability: quick boredom, a tendency to change jobs or start multiple projects and abandon them.
Problems in romantic relationships: impulsivity, lack of active listening, forgetfulness or disorganization that leads to misunderstandings.
🧠 Strengths and Positive Traits
Alongside these challenges, many people with ADHD possess qualities that, in the right circumstances, can become unique strengths.
High creativity: the ability for nonlinear thinking and rapid idea generation.
High energy: they excel in environments that require movement or multitasking.
Hyperfocus: they can become intensely focused on topics that interest them.
Positive risk-taking: an entrepreneurial or innovative spirit in challenging situations.
🔄 Coping and Management Techniques
For children:
A consistent daily routine and regular sleep schedule
Using a star chart or reward system to reinforce positive behavior
Providing a calm, low-stimulation environment without visual clutter
For adults:
Breaking large tasks into small, manageable steps
Using reminder and planning apps
Practicing meditation or mindfulness to manage impulsivity and stress
For parents:
Practicing patience and understanding your child’s different way of thinking
Receiving specialized education about ADHD
Focusing on your child’s strengths and boosting their self-esteem
💬 Success stories of people with ADHD
Many successful individuals in fields such as creativity, entrepreneurship, art, technology, and even politics have lived with ADHD. By accepting and managing it, they have been able to find their own path. Examples of inspiring figures:
Michael Phelps (Olympic swimmer)
Justin Timberlake (singer and actor)
Richard Branson (founder of Virgin)
🧭 Summary of This Section:
Living with ADHD is a challenging journey, but it is not impossible. Gaining an accurate understanding of the disorder, accepting it—both personally and by those around you—and using the right tools can lead to a fulfilling, independent, and successful life.
The role of parents, teachers, and society
Family / School / Culture
How can we support people with ADHD?
Accepting and managing ADHD is not solely the responsibility of the individual with the condition. The support system around the individual—from family and school to society and the broader culture—plays a crucial role in improving the quality of life for people with ADHD. The more understanding and supportive the environment, the faster and more sustainable the individual’s adaptation and progress will be.
👨👩👧 The role of parents: the main pillar of support for the child
✅ Understanding and acceptance:
ADHD is a neurodevelopmental disorder, not a behavioral choice.
Aggression or punishment toward the child is usually ineffective or even harmful.
✅ Creating a stable and structured environment:
Setting specific times for sleep, waking up, studying, and playing
Using visual checklists or daily schedules
✅ Encouragement and positive feedback:
Reinforcing good behaviors with small and immediate rewards
Focusing on small improvements instead of criticizing mistakes
✅ Active participation in treatment:
Cooperating with psychologists, teachers, and doctors
Attending parent training sessions or support groups
🏫 The role of schools and teachers: a determining factor in the educational journey
✅ Specialized teacher training:
Becoming familiar with the symptoms of ADHD and understanding how they differ from laziness or rudeness
Using structured classroom management techniques
✅ Effective educational interventions:
Allowing brief movement during class (such as standing up or holding a stress ball)
Using visual resources, videos, and a variety of exercises for teaching
Adjusting exam conditions (extra time, oral exams, use of assistive tools)
✅ Psycho-social support:
Preventing labeling or comparing the child to others
Boosting self-esteem by involving the child in school activities
🌍 The role of society and broader culture
✅ Raising public awareness:
Media campaigns to accurately introduce ADHD
Producing scientific content in simple language for schools, media, and social networks
✅ Reducing stigma:
Changing the stereotypical view of “hyperactive = rude” or “restless = disruptive”
Promoting understanding of neurological differences among people
✅ Legal support and policymaking:
Providing educational accommodations for students with ADHD
Including education about behavioral disorders in teacher training programs
Medication insurance and healthcare coverage for ADHD treatment
🧭 Summary of This Section:
| Group | Key Role | Effective Actions |
|---|---|---|
| Parents | Managing the home environment | Acceptance, providing structure, positive reinforcement |
| Teachers | Improving the educational experience | Adjusting conditions, diversity-focused teaching |
| Society | Shaping attitudes | Raising awareness, eliminating stigma, legal support |
🧩 Only through the collaboration of these three pillars can a healthy, safe, and nurturing path be created for individuals with ADHD.
The latest scientific findings and new technologies (2025)
Scientific advancements / digital tools / combination therapies / gut microbiome
How do knowledge and technology contribute to a better understanding and more effective management of ADHD?
The year 2025 can be considered a turning point in scientific and technological advancements related to Attention Deficit/Hyperactivity Disorder (ADHD). By combining neuroscience, digital technologies, and personalized medicine, new pathways have emerged for diagnosing, treating, and even preventing the worsening of ADHD symptoms.
🧬 1. Scientific advances in brain research and genetics
🔬 More precise brain imaging:
Use of high-resolution fMRI and MEG to observe abnormal brain activity patterns in affected individuals.
Enabling early detection of risk patterns at young ages.
🧬 Personalized genetics:
Analysis of genes associated with ADHD, such as DRD4 and DAT1 genes.
Using genetic tests to select the appropriate medication type and dosage.
🧠 These achievements enable physicians to design more personalized and precise treatments for each individual.
📱 2. Therapeutic apps and digital tools
In 2025, many complementary ADHD treatments are delivered digitally and interactively:
🧩 Attention and memory training apps:
EndeavorRx: the first FDA-approved video game for treating ADHD in children
CogniFit ADHD: cognitive training programs to improve focus, divided attention, and working memory.
⏰ Scheduling and organization apps:
Apps like Time Timer or BFT for teaching time management and reducing procrastination.
📊 AI-powered behavioral assessment platforms:
Analysis of a child’s motor and attentional patterns while playing with a tablet
Sending a report to the parent or psychologist in real time.
🧘♂️ 3. Focus on innovative combined and non-pharmacological therapies
🌿 Neurofeedback and Biofeedback:
Training the brain to regulate its brainwaves through real-time feedback.
Significant impact in reducing symptoms without the need for medication.
🧠 Brain stimulation (Neurostimulation):
New technologies such as tDCS (transcranial direct current stimulation)
Studies have shown that in some patients, it has led to increased focus and reduced impulsivity.
🍽️ 4. Nutrition and the gut microbiome
Studies in 2025 have found a strong relationship between gut microbiome health and brain function:
Probiotics and fiber-rich diets can help reduce ADHD symptoms.
The “gut-as-a-second-brain” hypothesis has been widely incorporated into combined ADHD therapies.
🧭 Summary of This Section:
| Domain | Innovations | Impact |
|---|---|---|
| fMRI neurology | personalized genetics | early diagnosis and targeted treatment |
| digital | game therapy, organizational apps | active child participation in therapy |
| Brain stimulation | neurofeedback, tDCS | alternative or adjunct to medication. |
| Nutrition | microbiome · Dietary therapy | More sustainable improvement from within |
Conclusion and Final Recommendations
Attention Deficit/Hyperactivity Disorder (ADHD) is more than just a psychiatric label; it reflects the diversity of human brain functioning. ADHD can affect a person’s life in many different ways, but with proper understanding, acceptance, support, and appropriate treatment, many of its challenges can be managed and even transformed into opportunities.
✅ Summary of key points
ADHD is a real, biological disorder, not laziness or lack of intelligence.
Its symptoms differ between children and adults yet remain persistent.
Accurate diagnosis requires a comprehensive evaluation by professionals.
Effective treatments include medication, behavior therapy, education, lifestyle modifications, and innovative technologies.
Living with ADHD is both challenging and full of opportunity, provided that the individual embraces acceptance and personal growth.
Parents, teachers, and the community each play a vital role in the path to recovery and flourishing of individuals with ADHD.
🎯 Final Practical Recommendations
If you notice ADHD symptoms in yourself or those around you, don’t self-diagnose; consult a specialist psychologist or psychiatrist.
Focus on your strengths; your creativity, energy, and unique perspective are true assets.
Help a child with ADHD to better understand themselves, rather than change to fit stereotypes.
Use reputable sources; be mindful of misinformation on social media.
If you’re a parent or teacher: offer support, not blame; foster understanding, not excessive control.
💡 Conscious Conclusion
In a world that increasingly respects neurodiversity, ADHD is not a deficit but a difference in brain functioning. When properly understood and supported, this difference can serve as a foundation for growth, creativity, and success.
References
Comprehensive ADHD Guide for Children and Adults – American Psychiatric Association (APA)
DSM-5 Diagnostic Guide – National Institute of Mental Health (NIMH)
Clinical and Statistical Information on ADHD – Centers for Disease Control and Prevention (CDC)
New scientific research on ADHD and the brain – Harvard Health
The role of genetics and brain imaging in ADHD – National Institutes of Health (NIH)
The role of the gut microbiome in psychiatric disorders such as ADHD – Frontiers in Psychiatry
Approval of the first digital therapeutic game for ADHD – EndeavorRx (FDA Approved)
Digital apps and tools for focus and organization – CHADD
Clinical guide to ADHD treatment – Mayo Clinic
2025 research on novel treatments – EatingWell Trends
Pelank Life | Body Health Assessment
The Best Body Health Calculators Using Scientific Methods
Developed by Pelank Life ©